Sci Transl Med:缓解炎症性肠病:一种颇具前景的新方法
2019-04-08 佚名 中国生物技术网
对于很多炎症性肠病患者来说,直接针对炎症的治疗方法基本上没有什么效果。近日一项研究表明,阻断参与凝血的蛋白质可能成为一种非常具有前景的替代疗法。
对于很多炎症性肠病患者来说,直接针对炎症的治疗方法基本上没有什么效果。近日一项研究表明,阻断参与凝血的蛋白质可能成为一种非常具有前景的替代疗法。
在分析了大量炎症性肠病(IBD)患者的遗传数据后,美国华盛顿大学医学院的研究人员发现,在那些症状最严重的患者体内,与凝血相关基因的活性也较高。这些活跃的基因既存在于炎症细胞也存在于上皮细胞中。
在研究中,因发现基因SERPINE-1与被其编码的蛋白质PAI-1尤其活跃,因此研究团队决定重点关注它们。已知PAI-1及其编码基因都参与凝血的早期阶段,但最近这项研究首次将它们与炎症关联起来,虽然只是间接关联。
研究人员发现,一种阻断PAI-1的实验性药物缓解了该疾病小鼠模型的IBD症状。这项研究近日已发表在《Science Translational Medicine》上。
研究通讯作者、实验室和基因组医学教授Thaddeus S. Stappenbeck博士说:“没有人会想到关注这个目标。但是,我们发现了一些可能对许多IBD患者有所帮助的东西,尤其是那些无法从当前疗法获益的患者。”
溃疡性结肠炎和克罗恩氏病美国疾病控制与预防中心(CDC) 2015年的数据显示,美国约有300万成年人被诊断患有溃疡性结肠炎或克罗恩病,这两种疾病构成了IBD。溃疡性结肠炎和克罗恩病的主要区别在于,溃疡性结肠炎的炎症主要影响结肠,而克罗恩病则可发生在胃肠道的任何地方。IBD症状主要包括腹痛、腹泻、体重减轻和疲劳。对于症状更严重的人,还会出现直肠出血和便血的情况。
标准疗法是给予皮质类固醇或其他药物以抑制炎症。然而,对于许多患有IBD的人来说,这要么不起作用,要么只是轻微缓解症状。
医生们还会用抑制免疫系统的强效药物治疗更严重的症状,包括那些阻断免疫蛋白TNF的药物。这些药物可以缓解症状,但并不总是有效的,而且也会增加患癌症和感染的风险。
新方向
Stappenbeck教授和他的团队并没有循规蹈矩地沿着针对炎症的方向寻找药物,而是决定另辟蹊径。
他们对可能导致IBD的基因进行了详细搜索,而这些基因并不与炎症直接相关。为了达到这一目的,他们对超过1800例IBD患者活检样本的基因数据进行了分析。
各种研究通过比较患有IBD和没有患有IBD的人的活组织切片得出了这些数据。来自IBD患者的活检包括来自炎症和非炎症肠道组织的样本,以及来自严重、中度和轻度疾病的样本。
正是这一分析产生了一系列基因都与凝血相关,而这些基因在IBD患者体内更加活跃。
这项发现支持了其他研究者曾经观察到的结果:IBD患者比非IBD患者出现凝血问题的风险高出2倍,尤其是在发病期间。
最终,研究团队将重点放在SERPINE-1及其蛋白PAI-1上,指出它们在炎症细胞和上皮细胞中都具有高度的活性,而且它们都参与了凝血的早期阶段。
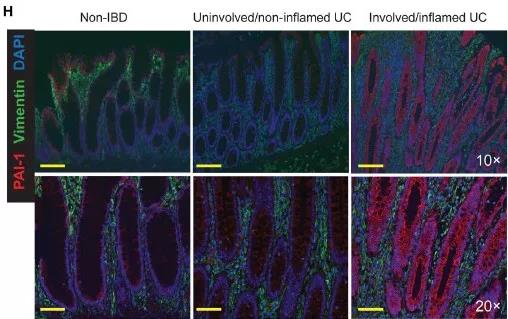
图片来源:《Science Translational Medicine》
Stappenbeck教授说:“最令人兴奋的是,SERPINE-1及其蛋白质似乎在患有最严重疾病的人和那些对免疫抑制生物制剂没有反应的人中表达最高。”
颇具前景的靶点
随后,Stappenbeck教授团队通过给小鼠一种在肠道中产生相同损伤和症状的化合物建立了IBD小鼠模型。
与该团队用无害化合物治疗的对照小鼠相比,IBD小鼠体重减轻,肠道组织出现病变,炎症蛋白和细胞水平升高,这与IBD症状一致。此外,IBD小鼠肠道组织中SERPINE-1的表达水平是对照组小鼠的6倍。
然后,研究团队使用MDI-2268(阻断PAI-1作用的一种实验药物)对部分IBD小鼠治疗,其余小鼠使用安慰剂。
与使用安慰剂的小鼠相比,服用实验药物的IBD小鼠开始出现健康改善的迹象:体重减轻的情况消失,肠道组织的病变与炎症也减少了。
Stappenbeck教授解释说:“我们发现了一个独特的靶点,它不是炎症分子,但阻止它可以减少炎症和疾病的迹象,至少对小鼠如此。如果进一步的研究证实了我们的发现,这将能帮助更多患者。”
研究团队认为,这一发现将为目前无法从现有疗法中得到缓解的IBD患者带来新的治疗方法。
Stappenbeck教授说:“人们对治疗IBD的新疗法很感兴趣,因为抑制炎症分子并不是对所有患者都有效。”
原始出处:Gerard E. Kaiko, Feidi Chen, Chin-Wen Lai, et al. PAI-1 augments mucosal damage in colitis. Sci Transl Med, 06 Mar 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TRA#
35
#Transl#
24
#新方法#
34
#炎症性#
23
#Med#
37