JACC:肺动脉高压相关发病率与患者的死亡风险呈明显相关
2018-02-24 MedSci MedSci原创
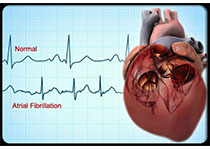
一般认为,疾病进展过程中出现肺动脉高压(PAH)是预后不好的征兆,然而,PAH相关发病率与预后的相关性没有在随机临床对照试验中证实。本研究的目的旨在用SERAPHIN 和GRIPHON临床研究的数据评估PAH发病事件对后续死亡风险的影响。在SERAPHIN研究中,出现有PAH事件患者3个月的死亡率要高于无PAH事件患者([HR]: 3.39; 95% [CI]: 1.94-5.92)。在GRIPH
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
46
#发病率#
30
#JACC#
38
#死亡风险#
36
#ACC#
36
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
38