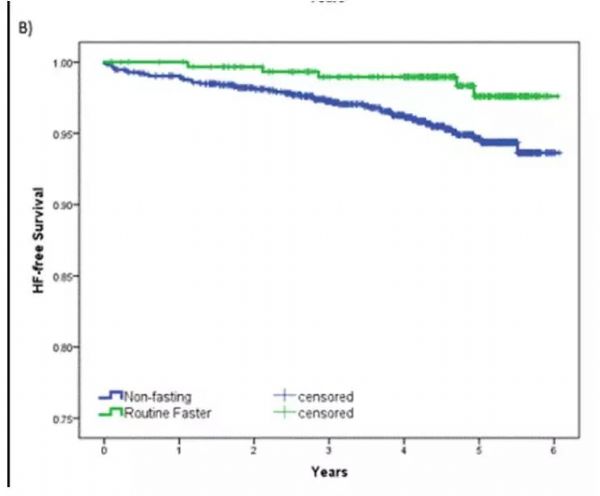
Nutri Metab Cardiovas:降低心衰风险、延长心血管疾病患者寿命,间歇性禁食益处多多!
2019-11-19 Paris 转化医学网
导语:间歇性禁食最初因“网红减肥法”而被大家所熟知,近些年更因为其可改善类风湿性关节炎、多发性硬化症以及糖尿病患者的病情而备受热议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病患者#
40
#间歇性#
30
#Meta#
31
#MET#
26
#心衰风险#
45
#血管疾病#
19