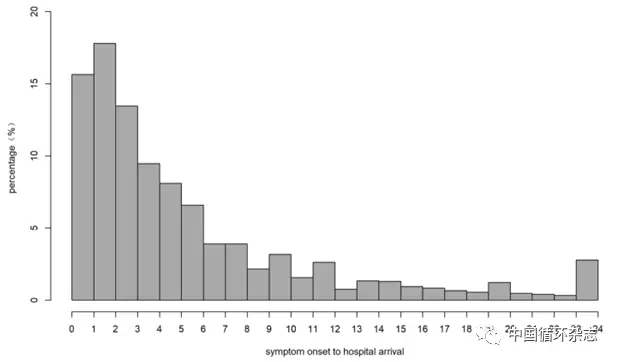
Eur Heart J Qual Care Clin Outcomes:中国心梗患者仅43%认为症状与心脏有关,一半没有及时就医
2018-06-12 卢芳 中国循环杂志
2010年,我国约有800万心梗患者,2030年将飙升到2300万。怎么救治心梗患者成了我国一个重要问题。能否尽快去医院就诊就是挽救生命的关键。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心梗患者#
19
#ART#
21
#HEART#
16
#MES#
36
学习了.谢谢分享
51
^_^^_^^_^
55
学习了.谢谢分享.
54