JACC:重度子痫前期患者的心功能临床研究
2018-06-27 MedSci MedSci原创
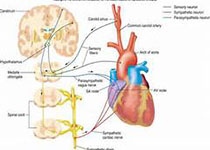
重度的子痫前期(PEC)患者会伴有严重的高血压和器官功能障碍,会增加短期的心血管不良事件风险。本研究的目的旨在评估PEC孕妇短期内的超声心动图、临床特征和实验室检查的变化,主要包括右室收缩压(RVSP)和心超相关的舒张期、收缩期和斑点追踪参数。本研究纳入分析了63名PEC孕妇和36名正常妊娠孕妇。分析结果显示,与对照组相比,PEC孕妇的RVSP更高(31.0 ± 7.9 mm Hg vs. 22.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
39
fcdrgws在
93
#ACC#
43
#子痫前期#
52
#心功能#
56
学习了.谢谢分享
65
学习了.谢谢分享!
82