lancet Oncol:来拉度胺不建议用于治疗转移性去势抵抗性前列腺癌
2015-03-03 姜英浩译 MedSci原创
目前在临床上,针对转移性去势抵抗性前列腺癌尚无有效的治疗方法。来拉度胺是一种抑制TNF-α分泌的小分子化合物,可作为免疫调节剂,具有抗血管生成的特性。因此,来自美国耶鲁肿瘤中心的Peytrylak教授领导开展了一项名为MAINSAIL的临床试验,试图探索来拉度胺与多西他奇(紫杉萜)和泼尼松联合使用在治疗初次化疗的转移性去势抵抗性前列腺癌患者的安全性及有效性。该结果在线发表于2015年3月3日的
目前在临床上,针对转移性去势抵抗性前列腺癌尚无有效的治疗方法。来拉度胺是一种抑制TNF-α分泌的小分子化合物,可作为免疫调节剂,具有抗血管生成的特性。因此,来自美国耶鲁肿瘤中心的Peytrylak教授领导开展了一项名为MAINSAIL的临床试验,试图探索来拉度胺与多西他奇(紫杉萜)和泼尼松联合使用在治疗初次化疗的转移性去势抵抗性前列腺癌患者的安全性及有效性。该结果在线发表于2015年3月3日的the Lancet Oncology杂志上。
在这项随机、双盲、安慰剂对照的3期临床试验中,研究人员招募初次接受化疗的进展性转移性去势抵抗性前列腺癌患者,将其按1:1的比例随机分为观察组和对照组。观察组在每个21天的治疗周期中第1-14天接受来拉度胺(25 mg)治疗;对照组则给予安慰剂。此外,两组受试者均于21天的周期内第1天接受多西他奇(75 mg/m2)和泼尼松(每2日5 mg)治疗。通过交互式话音应答系统完成置换区组随机化工作,并利用东部肿瘤协作组(Eastern Cooperative Oncology Group)评分、地理区域、疾病进展类型等进行分层工作。临床医生、患者及研究人员均对分组情况不知情。主要评估指标为整体生存率。通过意向治疗进行疗效分析。安全分析中包含了所有至少接受了1种研究药物治疗的患者。
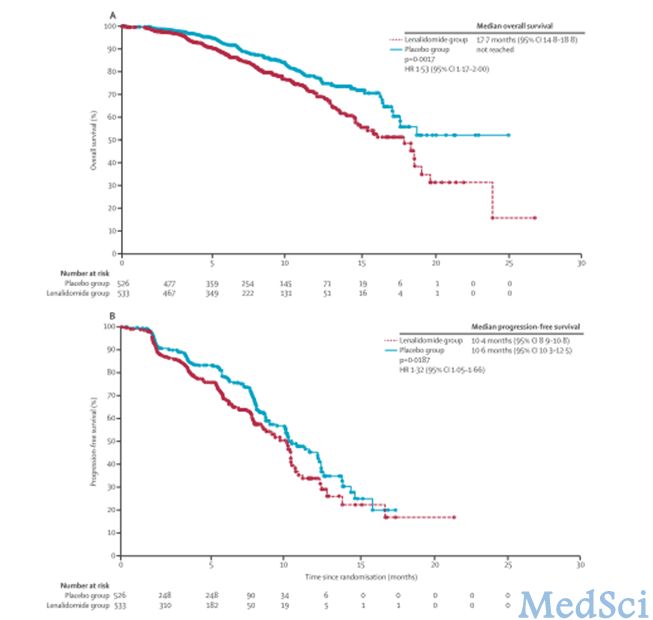
在该试验中,从2009年11月11日至2011年11月23日间,共有1059例符合条件的患者参与到了随机分组(观察组533例,对照组526例);其中1046例患者接受了治疗(观察组525例,对照组521例)。在8个月的中位随访期(IQR 5–12)后的数据截止时(2012年1月13日),共221例患者死亡:观察组129例,对照组92例。观察组的中位生存期为17.7个月(95% CI 14.8–18.8),未达到对照组的水平(HR 1.53, 95% CI 1.17–2.00, p=0.0017)。因此,该试验随后由于无效而被提前终止。关于治疗期间死亡数及最后给药28天内死亡数,2组之间无明显差异(观察组18/525, 3 %;对照组13/521, 2 %)。观察组有109例患者(21 %),对照组有78例患者(15 %)在最后给药28天以后死亡,主要原因是疾病进展。观察组有381/525例(73 %)出现了至少一次3级及以上副作用;对照组为303/521例(58 %)。其中3-4级嗜中性白血球减少症(观察组114例[22 %];对照组85例[16 %]);发热性中性粒细胞减少(62例[12 %];23例[4%]);腹泻(37例[7%];12例[2%]);急性肺炎(24例[5%];5例[1%]);呼吸困难(22例[4%];9例[2%]);无力(27例[5%];17例[3%]);肺栓塞(32例[6%];7例[1%])。观察组中各种副作用发生率均高于对照组。
根据以上试验结果,研究人员认为,在治疗转移性去势抵抗性前列腺癌时,在传统的疗法多西他奇(紫杉萜)与泼尼松联用时若加入来拉度胺共同治疗,治疗效果会显著降低。因此不建议批准未来关于此类联合治疗的后续研究。
临床试验注册号为:NCT00988208。
原始出处
Prof Daniel P Petrylak,Nicholas J Vogelzang,Nikolay Budnik,Pawel Jan Wiechno.et.al.Docetaxel and prednisone with or without lenalidomide in chemotherapy-naive patients with metastatic castration-resistant prostate cancer (MAINSAIL): a randomised, double-blind, placebo-controlled phase 3 trial. lancet Oncology.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
34
#Lancet#
23
#不建议#
38
#抗性#
24
很不错学习了
92
#去势抵抗性前列腺癌#
30
#转移性#
24
这是大样本数据!
92