葛均波院士完成世界首例深低温冷冻消融去肾动脉交感神经术
2015-11-04 心峰汇 心峰汇
2015年11月2日下午,中国科学院院士葛均波教授在复旦大学附属中山医院完成世界首例深低温冷冻消融去肾动脉交感神经术,这标志着国内心血管器械创新又一重大进步,有望为众多的顽固性高血压患者带来新的希望。 【首例临床概述】 深低温冷冻消融去肾动脉交感神经系统(CryoFocus) 是由中国人自主研发,具有独立知识产权的,全球首个专门用于肾动脉冷冻消融的导管系统。该系统以-68℃以下低温可
2015年11月2日下午,中国科学院院士葛均波教授在复旦大学附属中山医院完成世界首例深低温冷冻消融去肾动脉交感神经术,这标志着国内心血管器械创新又一重大进步,有望为众多的顽固性高血压患者带来新的希望。

【首例临床概述】
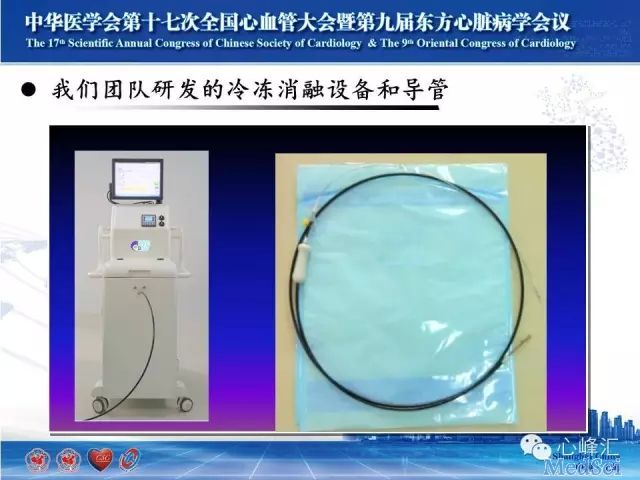
深低温冷冻消融去肾动脉交感神经系统(CryoFocus)
是由中国人自主研发,具有独立知识产权的,全球首个专门用于肾动脉冷冻消融的导管系统。该系统以-68℃以下低温可造成细胞不可逆损伤为理论基础,以液氮为制冷剂,通过冷冻球囊对肾交感神经进行消融。具有神经损伤完全,消融位置精确,血管内皮损伤小,不易导致血栓形成的特点。
今天治疗的是一位顽固性高血压的56岁男性患者,高血压病史10年,血压最高达210/120mmHg,先后多次调整药物,血压始终高于160/120mmHg,自3个月前起口服坎地沙坦8mg qd、阿罗洛尔10mg bid、乐卡地平10mg qd、氢氯噻嗪 12.5mg qd、螺内酯20mg qd,先后2次行动态血压监测,显示24小时平均血压约150/110mmHg。患者既往有房颤病史9年,有吸烟史,否认2型糖尿病史或冠心病家族史。入院查体心率绝对不齐,第一心音强弱不等,脉搏短绌,无其他显著阳性体征。甘油三酯6.38mmol/L,肾素5.76ng/ml,血管紧张素I1.06ug/L,血管紧张素II77.88pg/ml,醛固酮171.9pg/ml。入院后动态血压示:收缩压最高177mmHg,舒张压最高124mmHg,白天收缩压(>135mmHg)血压负荷值:75.5%,夜晚收缩压(>120 mmHg)血压负荷值:100%,白天舒张压(>85mmHg)血压负荷值:73.5%,夜晚舒张压(>70 mmHg)血压负荷值:93.3%。夜间平均血压147/95mmHg,白天平均血压144/94mmHg,全天平均血压145/94mmHg。心脏超声示:双房内径增大(左房内径51mm,右房上下径65mm),左室壁增厚(室间隔厚度14mm,左室后壁厚度13mm),轻度主动脉瓣反流。
2015年11月2日经股动脉穿刺行双侧肾动脉造影术,双侧肾动脉未见明显狭窄及血管畸形。在静脉滴注异丙酚全麻下行肾交感神经冷冻消融术。
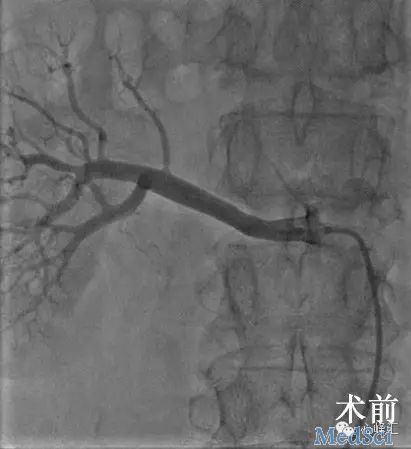
利用CryoFocus冷冻消融导管分别于左右肾动脉主支中段行冷冻消融3min,手术顺利。

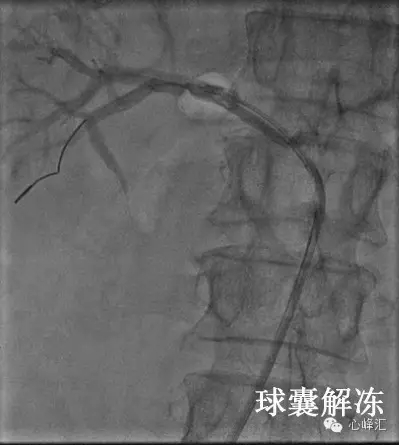

术后即刻复查造影双侧肾动脉未见血管夹层,血流通畅,无狭窄。术前血压170/90mmHg,术终血压130/70mmHg,心率60次/分,房颤律。术后患者无特殊不适。初步结果显示CryoFocus的手术可行性及安全性,其长期疗效将进一步随访。
目前正在进行FIM研究,第一期拟入组9例患者,随访时间6个月,主要评估该系统应用于顽固性高血压临床治疗的安全性及有效性。研究将由复旦大学附属中山医院和上海市第十人民医院共同完成。
【创新遇阻,勇于突破】
2014年初SYMPLICITY HTN-3试验以阴性结果告终后,给曾经红极一时的经导管肾动脉去神经术(RDN)前景蒙上了阴影。

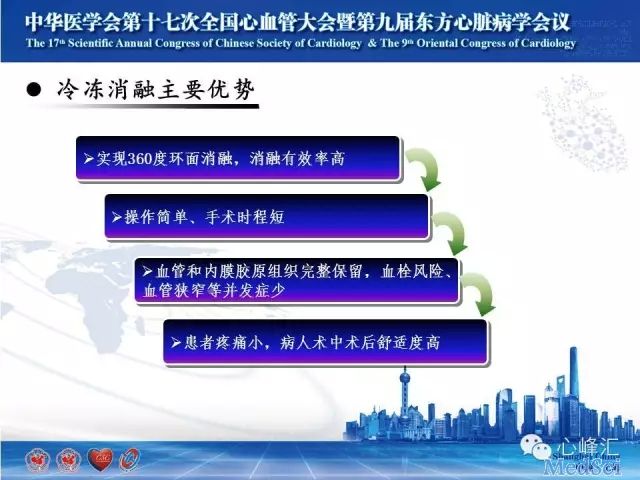
葛均波院士分析了以往器械可能存在的缺陷,并坚持探索新型的RDN系统,此次展示的冷冻消融导管系统有别于传统的射频消融导管,射频消融是逐点消融,消融切面不完全,而冷冻消融通过液氮作为冷冻载体,采用环面消融(360度消融),消融更加彻底,同时通过冷冻消融的内皮损伤更小,肾血管及周围组织修复快。

【坚持试验,突破难关】
动物实验证实,冷冻消融可以显著降低肾脏组织的去甲肾上腺素的分泌,最高降幅达90%,且神经损伤范围更均匀。

在临床前研究中该系统显示其功效优于传统的射频消融系统,若在下一步的临床研究中取得类似效果,将可能一举逆转RDN目前的颓势,成为新一代的RDN的主力产品。
中国心血管医生创新俱乐部(CCI)今年9月成立以来,“肾动脉交感神经冷冻消融导管系统”是第一个从俱乐部转化生产线上诞生的临床产品,其中集合了医生的创新理念和临床经验以及工程师的智慧和技术,两者通过历时三年的不断交流、探讨,尝试——失败——再尝试——再失败,直至最后产品成功应用于临床。
葛均波院士倡导的医疗器械的革新源于医生的创新理念再次得到印证,中国心血管医生创新俱乐部(CCI)将继续执着于实现中国医生的创新梦想,努力打造中国心血管医疗器械的“梦工厂”。

图为肾动脉交感神经冷冻消融导管系统创新团队合影
——————————————————
中国心血管医生创新俱乐部(CCI)
晓云感言:近年来,我国心血管介入医学领域不断有新技术、新成果涌现,并逐步获得国内外同行的认可,彰显出我国心血管介入医生创新实力不断提升。以历来重视创新性的东方会(OCC)为例,从2011年OCC播放国内首次经导管主动脉瓣置换术(TAVR)的手术录像、2012年实时转播亚洲首例经导管二尖瓣夹合术(Mitra Clip)、2013年直播国内首例经皮肺动脉瓣置入术(PPVI)、2014年国内首次直播经皮心室重建术(PVR)的手术演示、到今年OCC开幕式隆重启动,葛均波院士引领着心血管医生在国产创新道路上阔步前行。
我们也期待“肾动脉交感神经冷冻消融导管系统”更长时间的随访观察和深入研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好,不错,以后会多学习
73
#肾动脉#
36
#世界首例#
54
不愧成为国内心血管唯一一位院士
129
厉害
115
#消融#
33
#葛均波院士#
39
厉害呀
109