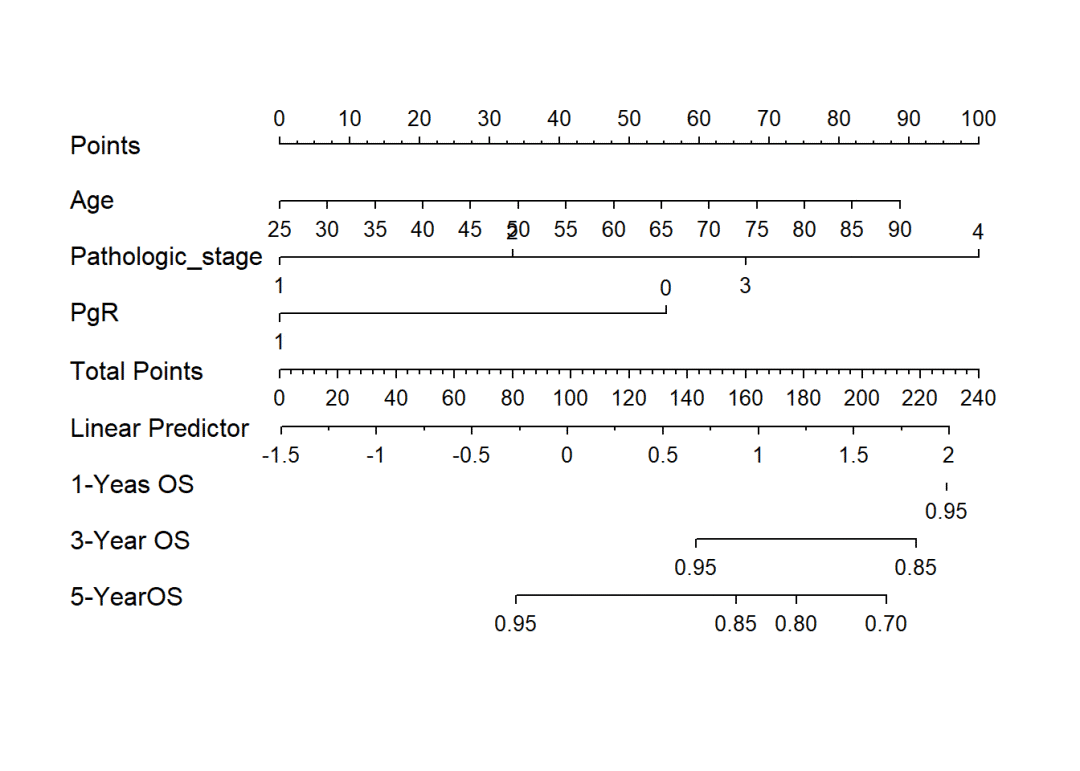
如何根据Cox回归Nomogram列线图计算所有患者的风险得分
2020-07-04 网络 网络
我们通过Cox回归等方法构建临床预测模型,然后根据模型参数把患者的生存概率可视化为Nomogram。“Nomogra”中文常翻译为诺模图或列线图,其本质就是回归方程的可视化。它
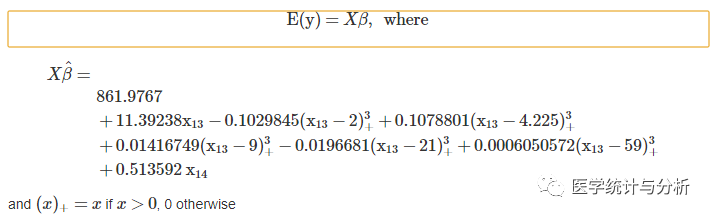
dd <- datadist(train) option <- options(datadist = "dd") coxm <- cph(Surv(Months,Status==1) ~ Age+Pathologic_stage+PgR, data = train, x = T, y = T, surv = T) surv <- Survival(coxm) nom <- nomogram(coxm,fun=list(function(x)surv(12, x), function(x)surv(36, x),function(x)surv(60, x)), lp = T,funlabel = c('1-Yeas OS', '3-Year OS','5-YearOS'), maxscale = 100, fun.at = c('0.95','0.85','0.80','0.70','0.6','0.5','0.4','0.3','0.2','0.1')) plot((nom), xfrac = .3) 我们通过Cox回归等方法构建临床预测模型,然后根据模型
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







专业
38
很好 很实用
37
专业
46
如何输入病人的相关参数,得出患者的生存率?
55
#列线图#
40
学习
81
#Nomogram#
42
#MOG#
31