跟距联合并胫后肌腱炎1例
2019-01-17 魏志勇 孙超 王智 足踝外科电子杂志
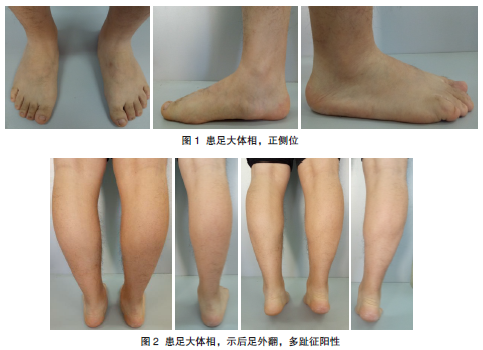
患者,男性,30岁,因“右足部内侧疼痛5年,疼痛渐加重2个月”来诊。患者5年前无明显诱因出现右足部内侧疼痛,发现右足弓内侧突起,因疼痛不激烈故未行干预。后逐渐出现疼痛明显,行走、运动及劳累后疼痛加重。疼痛为钝性,与负重及劳累有明确的关系,休息后缓解。2个月前患处疼痛较既往明显加重,严重影响患者运动及生活。查体:非负重状态下右侧足弓可,负重时足弓塌陷(图1),跟骨外翻,前足外展(图2),内踝下后内侧
跗骨联合为青少年期平足常见原因,常见为跟距联合,其次为跟舟联合。本文介绍1例跟距联合并胫后肌腱炎患者的治疗方法。
病历资料
患者,男性,30岁,因“右足部内侧疼痛5年,疼痛渐加重2个月”来诊。患者5年前无明显诱因出现右足部内侧疼痛,发现右足弓内侧突起,因疼痛不激烈故未行干预。后逐渐出现疼痛明显,行走、运动及劳累后疼痛加重。疼痛为钝性,与负重及劳累有明确的关系,休息后缓解。2个月前患处疼痛较既往明显加重,严重影响患者运动及生活。查体:非负重状态下右侧足弓可,负重时足弓塌陷(图1),跟骨外翻,前足外展(图2),内踝下后内侧可见骨性突起,胫后肌腱止点跖侧处压痛,内翻足部时可诱发该处疼痛,右外踝前下距下关节处压痛,距下关节僵硬。腓肠肌挛缩试验(Silverskioldtest)阴性(图3)。足背及胫后动脉搏动正常,足趾血液循环、感觉、运动正常。右足负重正侧位X线片示右足足弓扁平(图4)。

X线测量:第1、2跖间角11°,距骨第1跖骨角3°,距舟覆盖角23°,Meary角9°,Pitch角19°,跟骨外翻10°。双足负重CT示右足扁平改变,右跟距骨桥形成(图5)。诊断结果:右跟距骨性联合。明确诊断后,全身麻醉,患者取仰卧位,右下肢上止血带。首先松解腓肠肌,而后距跟联合探查:取内踝下方载距突上斜行切口长约5CM,切开皮肤,逐层分离皮下组织,于胫后肌腱与趾长屈肌腱之间进入,显露载距突部位及之后的关节面,以骨凿及骨膜剥离器先后探查,见距跟后关节面处存在紧密的骨性联合(图6A),不能探及联合间隙,反复活动距下关节,见后关节面距跟之间连接紧密,无相对活动。用骨刀逐步切除相连的骨桥(图6B),直至暴露出后跟距关节间隙,从足外侧跗骨窦插入一枚克氏针从内侧跗骨管穿出,显露跗骨管,清除跗骨管内的骨性联合部分,同时显露中跟距关节面,清除关节周围骨性联合(图6C),再次检查距下关节活动良好。

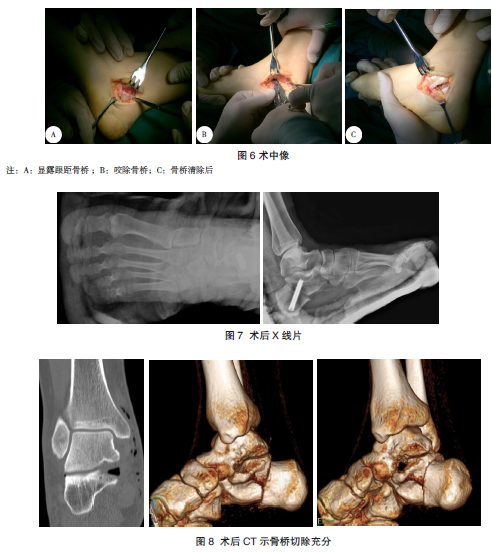
跟骨内移截骨手术:取跟外侧斜行切口,长约4CM,逐层分离皮肤及皮下组织,显露跟骨外侧壁。以宽摆锯于跟骨外侧壁斜行由后上至前下的斜行截骨,以骨膜剥离器及椎板撑开器反复撑开截骨面,保证两截骨断端完全分开,将跟骨结节部位骨块向内侧推移约1CM,取1枚直径为8mm×45mm的空心螺钉从足后跟经皮固定。“C”型臂透视确认内固定可靠,后足力线良好。胫后肌腱
探查:于原来的足内侧切口处,探查胫后肌腱,发现胫后肌腱因骨桥切除后松弛,予紧缩缝合。确认胫后肌腱于内踝后方走行区无张力。术后X线片示足部足弓恢复良好,内固定物在位(图7),三维CT提示跟距骨桥切除充分(图8)。术后石膏固定,4周后拆除石膏,行踝关节活动锻炼,前6周禁止下地负重活动。6周后患肢部分负重行走锻炼。
讨论
跟距骨桥或跟距骨性联合是跗骨联合的一种类型,指的是跟骨与距骨之间的异常骨性或纤维连接,并由此导致后足的活动受限。临床上,跟距骨桥的发病缺乏特征性,所以对于没有经验的医师,容易出现漏诊。
影像学检查 X线片检查X线检查包括足部负重正侧位平片和跟骨的长轴位片,能够发现骨化完全及部分骨化的跟距骨桥,对未骨化的跟距联合不敏感。Lateur描述侧位片上的“C”形征为跟距骨桥在侧位X线片可见距骨头和载距突边缘轮廓组成环状高密度影。以往观点认为“C”形征与跟距骨桥有相关性,但是也有学者认为C型征对跟距骨桥无敏感性和特异性,只对平足畸形有特异性。
CT检查CT检查仍然是诊断和评估跟距骨桥的标准。Herzenberg等在尸体标本上用冠状位的CT来评估跗骨联合,他们认为CT比其他方法更有优势,可以明确跟距骨桥的性质、累及病变的范围和程度,对于治疗方案的选择和疾病预后情况的判断有指导意义。本文作者认为,CT是跟距骨桥的诊断及评估的金标准。同时,Rozansky等于2009年提出了,应用三维CT技术对跟距骨桥进行分型,对手术有指导意义。根据跟距骨桥的性质、位置、关节面的走行方向将跟距联合分为5型:1型,Linear-直线型,占40.7%;2型,LinearwithPosteriorHooK-直线/后钩型,占16.7%;3型,Shingled瓦片型,占14.8%;4型,CompleteOsseous完全骨化型,占11.1%;5型,Posterior后关节面型,占16.7%。
MRI检查MRI通过轴位、冠状位和矢状位进行检查,可发现纤维骨桥和确诊周围关节病变情况。矢状位和轴位主要用于评估跟舟骨桥,冠状位则主要评估跟距骨桥。
治疗方法 保守治疗无症状的跟距骨桥可以保守治疗,不需特殊处理;有症状的骨桥应根据位置、范围、症状严重程度和关节退变程度个体化选择治疗方法。保守治疗是首选方法。如果疼痛症状持续或复发,则应用管型石膏制动3~6周。
手术治疗对于有症状的跗骨联合,手术治疗包括切除和关节融合两种。跟距骨桥手术治疗的原则如下:①若受累关节面积<50%、无周围关节退变、关节间隙无狭窄,可行单纯手术切除,保留距下关节活动度;②若受累关节面积>50%、后足力线外翻超过16°,有距下关节炎、周围关节正常,行距下关节融合术;③若除了骨桥外,还有周围关节退变,则行三关节融合术。我们报道的这例病例,患者受累的关节面<50%,关节间隙无明显狭窄,故选择手术切除治疗。
手术切除跟距骨桥需注意:骨桥切除面达关节面下2mm,保证跟距关节间隙(尤其是跗骨窦后方的跟距中后关节间隙)达5mm以上;若患足存在外翻畸形,距下关节活动受限,Shazly等主张骨桥切除术后行跟骨内移截骨或外侧柱延长。
本例患者亦合并有后足力线的外翻,故我们加做了跟骨内移截骨纠正外翻。同时,对于跗骨联合切除后,文献推荐使用趾短伸肌、骨腊、脂肪等进行填充预防骨桥复发。Shazly等推荐使用聚丙烯网片填充在骨表面中防止复发。
经验总结 首先,要正确认识跗骨联合的相关知识和概念,在工作中要提高警惕性,特别是存在距下关节疼痛、活动受限,并且合并有平足的患者就诊时,应予以认真体检,常规拍摄足部负重正侧位片及跟骨长轴位片,常规CT检查,对于高度怀疑纤维联合的患者需要MRI检查。只有在临床工作中提高警惕,逐渐积累经验,才能够准确诊断跗骨联合,避免漏诊。
综上所述,对于跟距骨桥的治疗,需要严格把握适应证,才能取得好的治疗效果。
原始出处:
魏志勇,孙超,王智;等;跟距联合并胫后肌腱炎1例;《足踝外科电子杂志》 2018年02期
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肌腱炎#
45
#肌腱#
55
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
71
谢谢分享,学习了
0