梅斯作为媒体参与AOSpine 2016年度收官之作:复杂脊柱畸形高级研讨会讲师团阵容
2016-12-09 MedSci MedSci原创
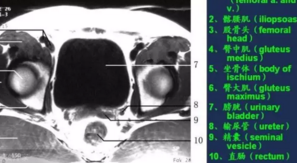
AOSpine 2016年度收官之作:复杂脊柱畸形高级研讨会讲师团阵容岳麓山下 群英荟萃2016.12.17 湖南长沙 敬请期待 不见不散由AOSpine中国区主办的复杂脊柱畸形高级研讨会,汇聚了国内外脊柱畸形领域的顶级和知名专家,是广大脊柱外科同道之不容错过的重要理由之一。在此组委会为您呈现他们的学术成就和风采。Kenneth Cheung 张文智 教授香港大学骨科学系主任、英国皇













本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研讨会#
35
#Spine#
43
文章不错,值得学习
78
不错不错!
68
#梅斯#
22
#畸形#
27
#脊柱畸形#
44