J Clin Invest:研究发现帮助对抗侵袭性乳腺癌的免疫细胞!
2017-08-22 枫丹白露 来宝网
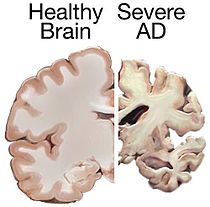
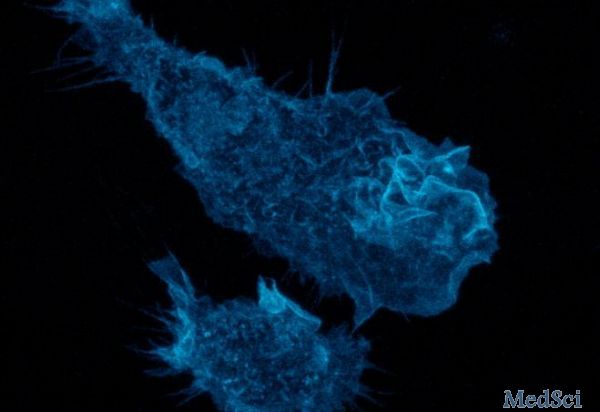
乳腺癌仍然是美国妇女与癌症相关死亡的主要原因。早期检测和靶向治疗改善了整体患者的疗效,但这些因素也深刻影响了预后。缺乏雌激素,孕激素和人类表皮生长因子2(HER2)激素受体表达的所谓“三阴”乳腺癌不能被现有的激素治疗所靶向,患者生存率差。三阴性乳腺癌的claudin-low亚型的特征在于其特异性较差的预后,以及肿瘤微环境中免疫细胞浸润的显著更高的速率。虽然观察结果表明,乳腺癌亚型中免疫浸润与患者预
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究发现#
32
学习
44
#EST#
34
#侵袭性乳腺癌#
24
#侵袭性#
28
谢谢分享.学习受益匪浅
57