Science:成像技术活体监测HIV的扩散过程
2015-10-10 佚名 生物谷
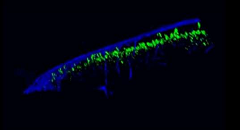
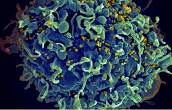
逆转录病毒(比如HIV)如何在宿主中进行扩散,目前科学家们并不清楚,近日,来自耶鲁大学的研究人员通过研究设计了一种方法,可以在活的有机体中实现对HIV扩散过程的观察,相关研究刊登在了国际杂志Science上,文章中研究者成功观察到了HIV如何到达并且在小鼠淋巴结中实现扩散的过程。研究者Walther Mothes教授说道,我们所观察到的病毒的扩散方式和人们想象中并不相同,实验中我们对小鼠机体中荧光
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#技术活#
35
#SCIE#
29
#成像技术#
32
感谢作者分享
109
动态成像发展迅速
47