Stroke:如何快速识别前循环颅内大血管闭塞的缺血性卒中患者?
2017-03-15 CSA&TISC 天坛会
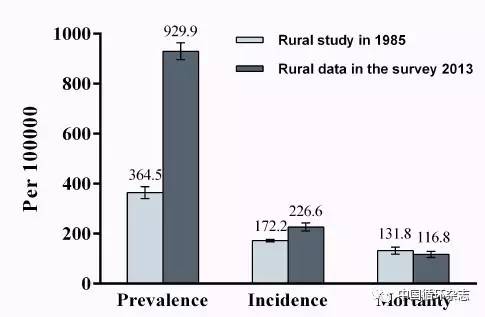
来自德国柏林卒中研究中心Scheitz JF等开展的一项前瞻性研究表明,通过简单改良的面-臂-语言-时间评分或评估NIHSS的症状表现可能有助于对前循环颅内大血管闭塞(LAVO)患者进行危险分层,并快速识别需要转移到综合卒中中心的患者。院前进行前瞻性测评是很有必要的。该项研究发表在Stroke杂志上。美国国立卫生研究院卒中量表(NIHSS)与前循环颅内大血管闭塞(LAVO)密切相关。因此,NIHS
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性#
31
#缺血性卒中患者#
35
#缺血性卒#
24
#血管闭塞#
32
#卒中患者#
35
#大血管#
31
凝视项很有提示意义
53