盘点:脑炎相关研究进展一览
2016-11-01 MedSci MedSci原创
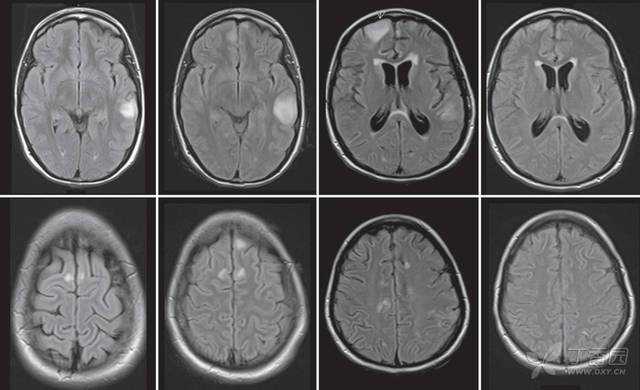
脑炎是一种严重的大脑炎性疾病,有许多可能的原因和复杂的鉴别诊断。自身免疫性脑炎过去10年的研究进展识别出了很多新的症状和生物标记物,改变了对此疾病的诊断方法。然而,精确诊断过度依赖于抗体检测和对免疫疗法的反应,可能会导致治疗延迟。梅斯医学小编就近期脑炎相关研究进展汇总,与大家分享。【1】新型自身免疫性脑炎—边缘性脑炎的研究进展边缘性脑炎(limbic encephalitis,LE)是一种新型
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#相关研究#
36
期待更多!
44
#脑炎#
34
#研究进展#
20
整理的内容很全面,学习了,临床使用价值也高
43
这个盘点不错~
37
学习一下!都是比较难诊断的脑炎!
41
谢谢~
42
真的学了很多
29