Nat Cell Biol:低剂量阿霉素或可克服白血病耐药性
2020-04-22 唐一尘 中国科学报
中美研究人员报告了一种或能克服白血病耐药性的新方法:使用低剂量的广泛用于治疗多种癌症的化疗药物阿霉素。
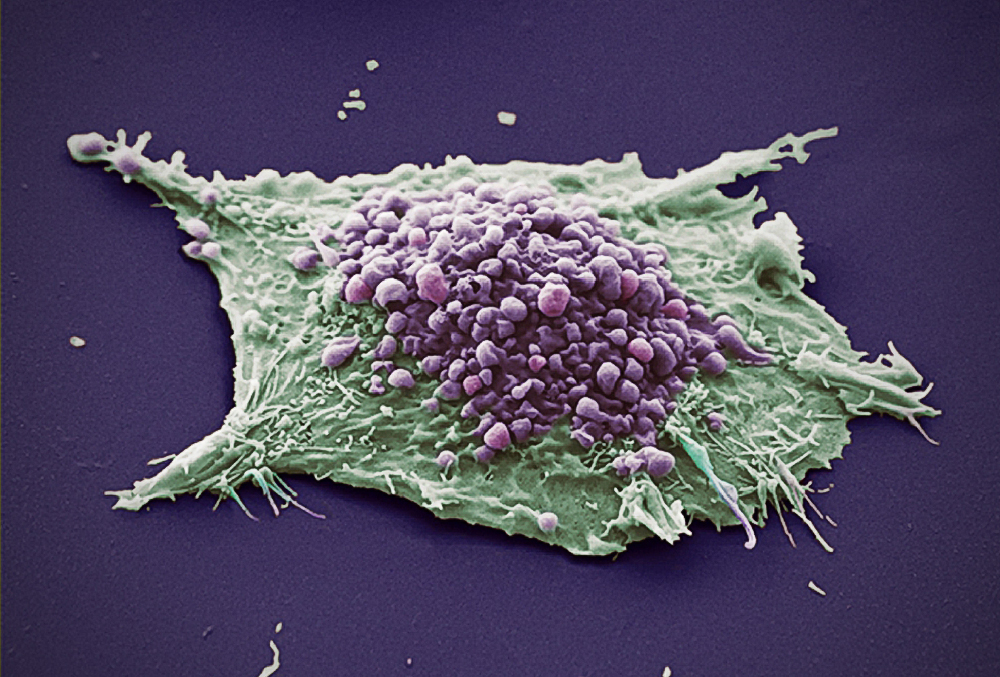
 低剂量阿霉素或可克服白血病耐药性。图片来源:《自然—细胞生物学》
低剂量阿霉素或可克服白血病耐药性。图片来源:《自然—细胞生物学》
4月20日在线发表于《自然—细胞生物学》的一项新研究中,中美研究人员报告了一种或能克服白血病耐药性的新方法:使用低剂量的广泛用于治疗多种癌症的化疗药物阿霉素。
针对癌症的传统化疗或放疗法虽然在治疗初期有一定的效果, 但所引起的耐药性往往导致癌症复发。近年来,抗免疫检查基因疗法(免疫疗法)成为了治疗癌症的新方法,但免疫疗法只在有限类型的癌症中显示出好的疗效,很大一部分患者仍在免疫治疗后复发。因此,包括免疫逃逸在内的抗药性的基本机制是亟待解决的根本问题。
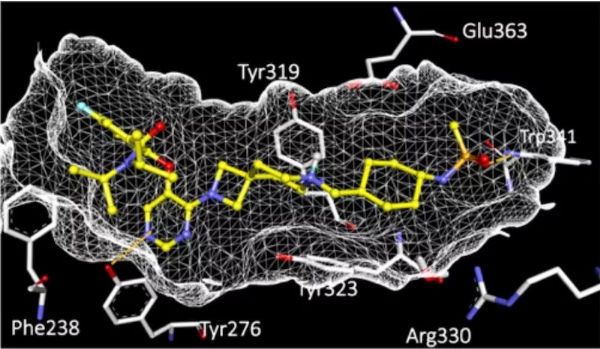
之前,研究人员假设,抑制β—连环蛋白的Akt磷酸化会降低前者的活性并抑制白血病。为了验证这一假设,美国Stowers 医学研究所、堪萨斯大学和中国清华大学等的研究人员,对美国食品药品监督管理局批准的化学文库进行了高通量筛选,并鉴定了24种先导化合物。结果发现广泛使用的化学治疗药物阿霉素特异性地以低剂量抑制Akt和β—连环蛋白的相互作用。
研究人员将低剂量阿霉素与临床使用的化学治疗剂奈拉滨一起用于治疗双突变小鼠。他们观察到化学疗法可有效消除占多数的白血病细胞,但诱导在数目上占少数的白血病干细胞的扩增。相反,低剂量阿霉素对白血病细胞没有影响,但减少了白血病干细胞。低剂量阿霉素和奈拉滨的组合治疗效果最佳。为了进一步确证抑制作用,研究人员合作进行了一项小型临床试验,以测试10到20例已对化疗产生耐药性的急性髓系白血病患者对柔红霉素的反应。结果表明,50%的已有化疗耐药性的急性髓系白血病患者对低剂量柔红霉素有反应,并显著降低了其白血病干细胞的数量。
研究还发现低剂量阿霉素针对白血病干细胞的抑制作用依赖于对抗癌表达CD8的T细胞。因此,新的治疗方法不仅直接针对白血病干细胞,还将它们暴露于激活的免疫反应中。
原始出处:
John M. Perry, Fang Tao, Anuradha Roy, et.al. Overcoming Wnt–β-catenin dependent anticancer therapy resistance in leukaemia stem cells. Nature Cell Biology 20 April 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Bio#
31
#Cell#
32
#Nat#
24
#Biol#
22
#CEL#
32
#低剂量#
17