Sci Rep:突破!利用CRISPR-Cas9技术开发出帕金森疾病新型筛选工具
2017-06-07 生物谷 生物谷
近日,一项发表在国际杂志Scientific Reports上的研究报告中,来自中佛罗里达大学(University of Central Florida)的研究人员通过研究利用突破性的基因编辑技术开发出了一种帕金森疾病的新型筛查工具,帕金森疾病是一种严重的神经系统疾病,这种技术能够帮助科学家们在实验室中对名为α-突触核蛋白的大脑蛋白进行实
近日,一项发表在国际杂志Scientific Reports上的研究报告中,来自中佛罗里达大学(University of Central Florida)的研究人员通过研究利用突破性的基因编辑技术开发出了一种帕金森疾病的新型筛查工具,帕金森疾病是一种严重的神经系统疾病,这种技术能够帮助科学家们在实验室中对名为α-突触核蛋白的大脑蛋白进行实时监测,这种蛋白和帕金森疾病发病直接相关。
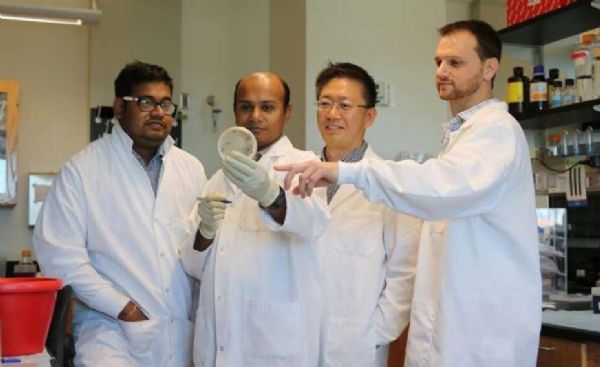
图片来源:UCF, College of Medicine
研究者Levi Adams说道,正常情况下,α-突触核蛋白存在于大脑中,但由于某些原因,有时候机体帕金森的水平会处于异常状态,因此如果我们能够对细胞中α-突触核蛋白的水平进行实时监测的话,我们就能够鉴别出引发这种蛋白水平异常的原因,并且采取措施及时应对。研究人员认为,本文研究工作对于后期开发治疗帕金森疾病的新型靶向性疗法非常关键。
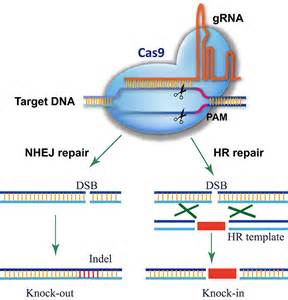
文章中,研究人员利用CRISPR-Cas9基因编辑技术进行研究,这种系统是科学家们近年来使用最为广泛的生物医学工具,其能够帮助科学家对植物和动物机体中的DNA进行精准化修饰,同时还不会杀灭正常细胞,如今这种新型的基因编辑系统慢慢地开始被研究人员用来开发治疗癌症和帕金森等疾病的新型疗法了。
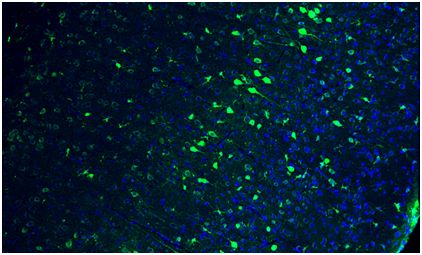
CRISPR-Cas9基因编辑技术能够对活体细胞中的DNA进行改变,同时其在不杀灭细胞的情况下还能够实时对基因表达进行监测,如果没有这种新型基因编辑技术,我们可能会从细胞中提取出所有的蛋白质来对其测定,这无疑会对细胞产生杀灭作用。这项研究中,研究者Burnett及其同事利用CRISPR技术对α-突触核蛋白基因进行了编辑,并且在该基因中插入了一种荧光标记,每当细胞开始产生α-突触核蛋白时,荧光标记就会发光;而这种反应就能够被研究者们轻松观察到,研究者Adams说道,发光越多就意味着α-突触核蛋白的水平增加越明显,这时候我们就要考虑是否个体已经处于疾病状态了。
研究者发现,对光进行测定时一种测定α-突触核蛋白产量的可靠方法;如果利用特殊药物来处理任何一个被修饰的细胞,如果细胞不再产生荧光,那就意味着这种药物或许能够用来治疗疾病。对细胞进行工程化修饰后,研究者就能够对新型和当前已经存在的药物进行筛选来观察期如何调节患者机体中α-突触核蛋白的水平。
未来研究人员希望能够通过更为深入的研究鉴别出新方法来降低α-突触核蛋白的产生,从而有效抑制帕金森疾病的发生和进展;本文研究中研究者重点对帕金森疾病发生期间α-突触核蛋白如何杀灭神经元进行了深入研究。
原始出处:
Sambuddha Basu, Levi Adams, Subhrangshu Guhathakurta, et al. A novel tool for monitoring endogenous alpha-synuclein transcription by NanoLuciferase tag insertion at the 3′end using CRISPR-Cas9 genome editing technique. Scientific Reports (2017) doi:10.1038/srep45883
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CRISPR#
26
#CRISPR-Cas9#
37
#Cas9#
36
#帕金森疾病#
0
#CRISPR-Cas#
32
#筛选#
23
#Cas#
32
是挺新颖的,可行性大吗
55
学习了谢谢分享。
63