JAMA Pediatr:冠状病毒在妊娠期的传播虽罕见,但确有发生!
2020-03-28 王昭月 生物探索
近日,中国科学家在《JAMA Pediatrics》发表研究指出,患COVID-19疾病的孕妇有可能将病毒传染给新生儿,这种情况很少见但确有发生。
随着COVID-19感染人数的急剧增多,确诊的孕妇和儿童人数也不断增加,但关于新生儿早期感染的研究却少之又少。近日,中国科学家在《JAMA Pediatrics》发表研究指出,患COVID-19疾病的孕妇有可能将病毒传染给新生儿,这种情况很少见但确有发生。
研究者对2020年1月至2月33名武汉儿童医院的孕妇进行追踪检查。其中,有关人口学、流行病学和临床特征的数据是从病案系统中获得的,用鼻咽和肛管拭子作了SARS-CoV-2的PCR荧光诊断检测,所有数据均用StataCorp进行统计分析。结果发现3例COVID-19新生儿,33例新生儿中有4例表现出气短症状,X射线表现无异样,且无死亡报告。
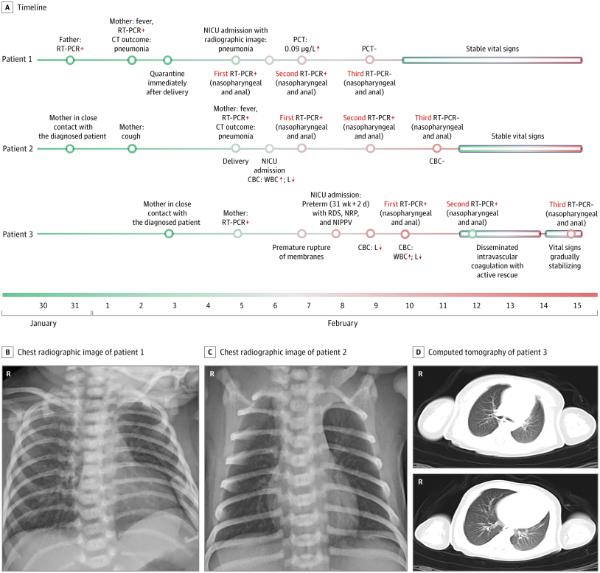
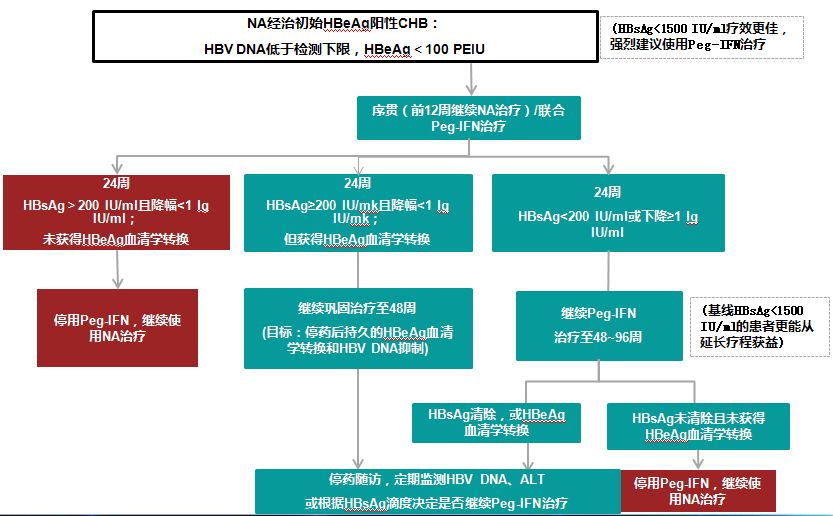
3例感染COVID-19新生儿的时间线及影像学表现
33名婴儿中有3名(9%)出现了早期SARS-CoV-2感染,且均为男性。两名按时分娩(妊娠40周、妊娠40周又4天)的新生儿经历了昏睡和发烧,两人均在重症监护室接受治疗,第六天SARS-CoV-2试验被检测为阴性。另一个婴儿为早产儿(妊娠31周又2天),被诊断患肺炎、呼吸急促和脓毒症,在重症监护病房接受治疗,第七天其SARS-CoV-2检测结果显示为阴性。
因分娩期间实施了严格的感染控制和预防措施,所以研究者推测新生儿上呼吸道或肛门中SARS-CoV-2的来源可能是产妇。尽管最近的2项研究表明,感染COVID-19的母亲所生的新生儿中没有任何临床表现或调查表明感染了,且包括羊水、脐带血和母乳在内的所有样本均为SARS-CoV-2阴性,但不能排除本研究中母婴垂直传播的可能性。因此,必须对孕妇进行筛查,采取严格的感染控制措施,隔离受感染的母亲,并密切监测感染COVID-19的新生儿。
原始出处:Lingkong Zeng, Shiwen Xia, Wenhao Yuan, et al. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. JAMA Pediatr. March 26, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#DIA#
48
#PE#
39
#妊娠期#
32
#罕见#
41
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
53