Heart:感染性休克患者右心室功能障碍与预后不良之间的关联
2020-07-23 MedSci原创 MedSci原创
三分之一的感染性休克患者表现出各种心肌功能障碍。左室收缩功能不全较为常见的。然而,只有RV功能障碍与短期死亡率有关。
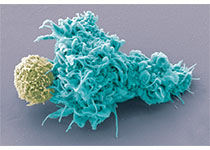
脓毒症引起的心肌功能障碍(SIMD)可以累及左右心室。但是,SIMD各种表现形式的特征和结局尚未明确。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,这是一项回顾性队列研究,研究人员使用了2011年1月至2017年4月期间感染性休克前瞻性登记中心数据。入院后72小时内研究人员将临床上推测为心脏功能障碍的患者进行了超声心动图检查,并招募入组(n=778)。SIMD分为左心室(LV)收缩/舒张功能障碍和右心室(RV)功能障碍,这是根据美国超声心动图学会标准定义的。该研究的主要结局为28天死亡率。
778名接受超声心动图检查的感染性休克患者中,有270名(34.7%)患者为SIMD。中位年龄为67.0岁,男性为主(57.3%)。其中,LV收缩功能障碍占67.3%,RV收缩功能障碍占40.7%,LV舒张功能障碍占39.3%。尽管两组之间的血清乳酸水平和顺序器官衰竭评估得分没有显著差异,但SIMD组肌钙蛋白I水平较高(0.1 vs. 0.1 ng/mL;p=0.02)和临床结局较差,包括较高的28天死亡率(35.9 vs. 26.8%;p<0.01),重症监护病房住院时间更长(5 vs. 2天; p<0.01)和机械通气时间延长(9 vs. 4天;p<0.01)。多变量分析表明,孤立的RV功能障碍是28天死亡率的独立危险因素(OR为2.26,95%CI为1.04至4.91)。
由此可见,三分之一的感染性休克患者表现出各种心肌功能障碍。左室收缩功能不全较为常见的。然而,只有RV功能障碍与短期死亡率有关。
原始出处:
June-sung Kim.et al.Association between right ventricle dysfunction and poor outcome in patients with septic shock.heart.2020.https://heart.bmj.com/content/early/2020/07/21/heartjnl-2020-316889
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#感染性#
38
#右心室功能#
39
#ART#
30
#功能障碍#
0
#预后不良#
34
#右心室#
33
#HEART#
32
#右心室功能障碍#
42
脓毒症引起心功能障碍
90
学习了
82