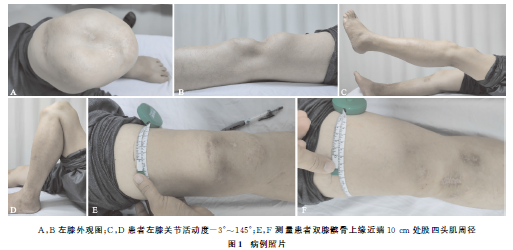
陈旧性髌骨骨折罕见病例1例
2019-02-25 童彬浚 高大伟 吴洪, 中国中医骨伤科杂志
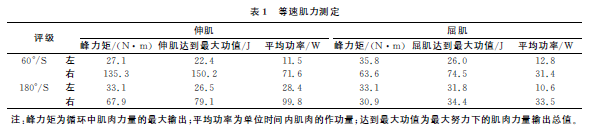
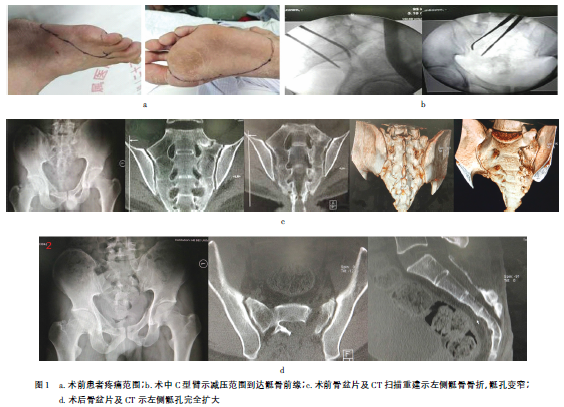
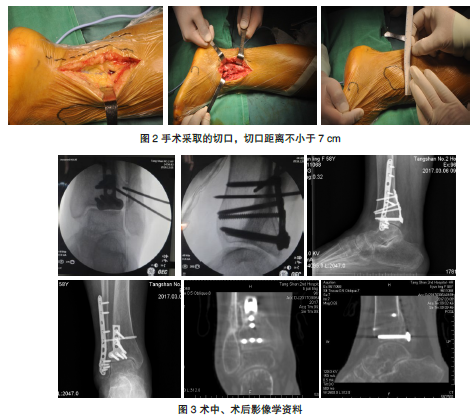
髌骨骨折是常见的骨科创伤疾病,常伴发髌骨周围韧带及支持带的损伤,后期可继发髌股关节骨性关节炎和伸膝装置效能降低。有研究认为髌骨能通过杆杠作用使股四头肌的力量增强30%,对于髌骨骨折一般要求尽量保留并恢复髌骨完整性,本例患者诊断为陈旧性髌骨骨折,受伤后未行手术治疗,10年随访,患者仍有较好的伸膝肌力,行走正常。对于髌骨骨折临床治疗中采取保守治疗的可行性分析,需要进行严谨的临床研究,本病例较为罕见,现

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#髌骨骨折#
76
#罕见病例#
33
已阅
66
#髌骨#
49
#罕见#
38
#陈旧性#
43