BMJ:85岁女性剧烈腹痛原因是啥?-案例报道
2016-11-17 xing.T MedSci原创
CT扫描显示肝内广泛的外周分支状气体,这与门静脉气体的诊断一致,该病例继发于小肠缺血。
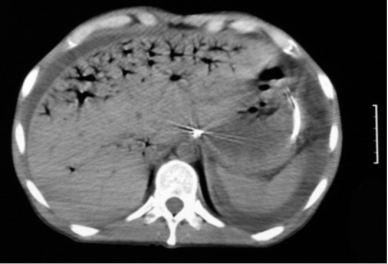
患者85岁,女性,因腹部僵硬、轻度肿胀伴剧烈腹痛而入院,患者肠鸣音消失。该患者还有房颤和低血压病史。该患者进行腹部CT扫描,其结果显示了啥(图1)?
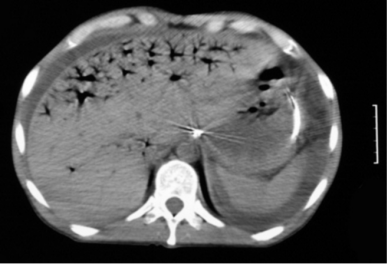
图1
答案:
CT扫描显示肝内广泛的外周分支状气体,这与门静脉气体的诊断一致,该病例继发于小肠缺血。
讨论
非增强CT扫描(图2)显示肝门静脉系统(P)内广泛的外周分布着分支状气体,这就被称为门静脉气体或肝门静脉气体。CT扫描也显示肝脏和脾脏周围存在液体(F),也可以看到放置在胃中的鼻饲管。
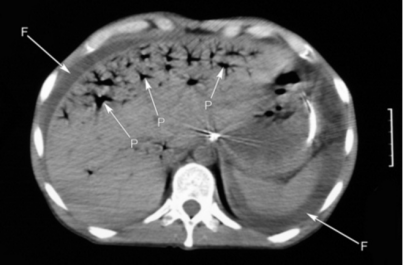
图2 腹部CT显示存在于肝门脉系统的气体。图像还显示肝脏、脾脏周围的液体,以及在胃中的鼻饲管。
门静脉气体的主要原因是缺血和脓毒症。该病例小肠缺血得到了证实。门静脉气体很少由其他病因引起,如全肠道扩张或炎症性肠病。
目前,门静脉气体形成的机制还没有完全理解。器官内气体形式可能是腔内气体通过结肠壁进入器官和静脉内微生物产生的气体二者相结合,肠壁的改变被认为可易化这一过程。
当肝内可见气体,应注意与胆管积气(气体位于胆道系统内)作鉴别诊断。胆管积气往往发生在经内镜逆行胰胆管造影术后,或在Oddi的括约肌功能不全。这是区分胆管积气和门静脉积气的重要指标,因为它们有着不同的原因。放射科医生通过气体位于肝脏中央还是外周来鉴别者两种疾病。在胆管积气中,气体位于中央因为被流动的胆汁推向肝脏中央。相反,门静脉积气可被血流推向外周。除了气体的分布不同,临床病史和继发性CT检查结果,如肠缺血、败血症或脓肿,有助于作出正确的诊断。
最后,该患者不适合手术治疗。
原始出处:
Joseph Dalby Sinnott,et al. Severe abdominal pain in an 85 year old woman. BMJ.16
November 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
门静脉气体的主要原因是缺血和脓毒症。该病例小肠缺血得到了证实。门静脉气体很少由其他病因引起,如全肠道扩张或炎症性肠病。
目前,门静脉气体形成的机制还没有完全理解。器官内气体形式可能是腔内气体通过结肠壁进入器官和静脉内微生物产生的气体二者相结合,肠壁的改变被认为可易化这一过程。
当肝内可见气体,应注意与胆管积气(气体位于胆道系统内)作鉴别诊断。胆管积气往往发生在经内镜逆行胰胆管造影术后,或在Oddi的括约肌功能不全。这是区分胆管积气和门静脉积气的重要指标,因为它们有着不同的原因。放射科医生通过气体位于肝脏中央还是外周来鉴别者两种疾病。在胆管积气中,气体位于中央因为被流动的胆汁推向肝脏中央。相反,门静脉积气可被血流推向外周。除了气体的分布不同,临床病史和继发性CT检查结果,如肠缺血、败血症或脓肿,有助于作出正确的诊断。
最后,该患者不适合手术治疗。
原始出处:
Joseph Dalby Sinnott,et al. Severe abdominal pain in an 85 year old woman. BMJ.16
November 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#BMJ#
31
很不错的病例
61
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
48
值得学习。
66
#腹痛#
40
好好看下
57