肠梗阻肠切除术后 患者缘何出现精神症状?
2017-08-17 佚名 环球医学资讯
Wernicke脑病是由各种原因引起的维生素B1缺乏而伴发的营养障碍性神经病,一般多累及丘脑、下丘脑、乳头体、第三脑室壁、中脑导水管周围灰质以及第四脑室底部,常为对称性病变。本文报告1例因肠梗阻肠切除后伴发的Wernicke脑病。
Wernicke脑病是由各种原因引起的维生素B1缺乏而伴发的营养障碍性神经病,一般多累及丘脑、下丘脑、乳头体、第三脑室壁、中脑导水管周围灰质以及第四脑室底部,常为对称性病变。本文报告1例因肠梗阻肠切除后伴发的Wernicke脑病。
临床资料
患者女性,49岁,主因“腹痛、腹胀、恶心、呕吐伴停止排气、排便10天”于2008年2月18日入院。3周前因“肠梗阻”在外院行手术治疗,具体不详。查体见:痛苦病容,腹部饱满,未见肠型及蠕动波。腹软,中上腹及脐周压痛,无反跳痛,未触及包块。叩诊鼓音,无移动性浊音。肠鸣音活跃。立位腹部平片显示胃潴留,空肠扩张,腹部CT未见占位。诊断为“粘连性肠梗阻”,给予营养支持及胃肠减压等。但患者症状缓解不明显,反复立位腹部平片显示梗阻水平位于第2组小肠附近,于2008年3月10日在全麻下行剖腹探查、空肠部分切除、小肠端端吻合术,肠切除约50cm,术后病理提示:肠腔明显狭窄,周径约4cm,可见肠套叠。2008年3月24日患者出现全身乏力,精神差,夜间偶有精神症状,伴有视幻觉,步态不稳及双下肢疼痛。查体见:淡漠,言语流利,应答基本切题,记忆力明显减退,计算力差,不能计算出100-7=?,双眼外展位,内收不充分,双眼可见水平及垂直粗大眼震,四肢肌力4级,腱反射(+),未引出病理反射。双下肢痛觉过敏。双侧指鼻及跟膝胫欠稳准。查头颅MR见双侧脑干及丘脑两侧对称性异常信号(图3.4‐1)。脑电图检查显示:中度异常,额颞叶为著。诊断:Wernicke脑病,肠梗阻术后。给予大剂量B族维生素及神经保护药物等治疗,7天后患者症状明显缓解,10天后上述症状基本消失,查体未见神经系统阳性体征。
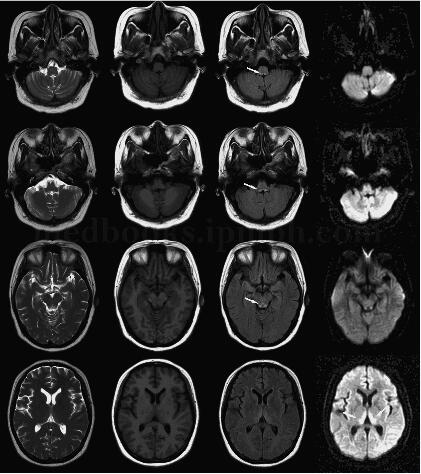
患者女性,49岁,主因“腹痛、腹胀、恶心、呕吐伴停止排气、排便10天”于2008年2月18日入院。3周前因“肠梗阻”在外院行手术治疗,具体不详。查体见:痛苦病容,腹部饱满,未见肠型及蠕动波。腹软,中上腹及脐周压痛,无反跳痛,未触及包块。叩诊鼓音,无移动性浊音。肠鸣音活跃。立位腹部平片显示胃潴留,空肠扩张,腹部CT未见占位。诊断为“粘连性肠梗阻”,给予营养支持及胃肠减压等。但患者症状缓解不明显,反复立位腹部平片显示梗阻水平位于第2组小肠附近,于2008年3月10日在全麻下行剖腹探查、空肠部分切除、小肠端端吻合术,肠切除约50cm,术后病理提示:肠腔明显狭窄,周径约4cm,可见肠套叠。2008年3月24日患者出现全身乏力,精神差,夜间偶有精神症状,伴有视幻觉,步态不稳及双下肢疼痛。查体见:淡漠,言语流利,应答基本切题,记忆力明显减退,计算力差,不能计算出100-7=?,双眼外展位,内收不充分,双眼可见水平及垂直粗大眼震,四肢肌力4级,腱反射(+),未引出病理反射。双下肢痛觉过敏。双侧指鼻及跟膝胫欠稳准。查头颅MR见双侧脑干及丘脑两侧对称性异常信号(图3.4‐1)。脑电图检查显示:中度异常,额颞叶为著。诊断:Wernicke脑病,肠梗阻术后。给予大剂量B族维生素及神经保护药物等治疗,7天后患者症状明显缓解,10天后上述症状基本消失,查体未见神经系统阳性体征。
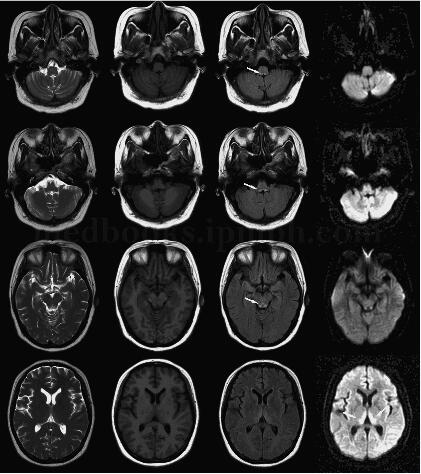
图3﹒4‐1头颅MRI
讨论
维生素B1是葡萄糖代谢过程中必需的辅酶,也是神经细胞膜的主要成分,而它在体内并无储存能力,所以长期酗酒、神经性厌食、胃大部切除术后、长期透析的患者均可出现维生素B1缺乏,造成有氧代谢障碍和神经细胞变性坏死,引起Wernicke脑病。
其病理改变主要包括脱髓鞘、水肿、毛细血管显著扩张、点状出血、血管内皮细胞增生、星形细胞肿大和胶质增生、神经核团大量空泡样变性及神经元坏死。导水管周围、中脑、顶盖、第三、四脑室旁、乳头体、丘脑为最常见的部位。
Wernicke脑病多呈急性或亚急性起病,典型的临床表现为眼肌麻痹、共济失调及精神障碍三联症,但相当多的病例仅表现一到两种症状,单表现为精神异常时易误诊为精神病。如果出现记忆障碍、学习不能、定向不能、淡漠、虚构为特征的临床表现时为Wernicke‐Korsakoff综合征。
MR的T1加权像呈低信号,T2加权像呈高信号。急性期弥散加权像呈高信号,ADC明显下降。如增强扫描可有明显强化或不强化。此外,小脑齿状核、脑桥被盖、红核、尾状核及大脑皮质也偶可累及。
本病主要用大剂量维生素B1治疗,同时积极纠正酸碱失衡及离子紊乱,多数症状可迅速好转。因葡萄糖可降低丙酮酸脱氢酶的活性,使丙酮酸无法进入三羧酸循环氧化供能,引起血中丙酮酸浓度增高出现精神及神经症状,而激素又能阻碍丙酮酸氧化,所以在未用维生素B1治疗前,禁忌静脉输糖及激素,否则会使病情进一步加重。
本病例考虑为肠切除过长,追查手术史,两次手术共计切除肠管近1m,引起维生素B1吸收障碍。发病后大剂量补充B族维生素,症状迅速改善,也支持本病的诊断。因而当双侧丘脑或中脑导水管周围出现异常高信号病变,且临床症状相似时需想到Wernicke脑病的可能。
原始出处:
《神经科少见病例》作者:张微微 戚晓昆页码:146-149出版:人民卫生出版社
《神经科少见病例》作者:张微微 戚晓昆页码:146-149出版:人民卫生出版社
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#精神症状#
50
#切除术#
31
学习了很多先进的技术水平
53
继续学习中谢谢
50
#肠梗阻#
23