Sagliker综合征患者甲状旁腺切除术麻醉一例
2019-11-25 李琳琳 张春璐 陈鹏 临床麻醉学杂志
患者,男,40岁,58 kg,因骨痛伴甲状旁腺激素升高19个月入院。高血压病史7年,最高达190/100 mmHg。6年前因“慢性肾功能衰竭(尿毒症期)”开始规律血液透析,2年前出现骨痛症状,19个月前发现甲状旁腺激素升高,约3 600 Pg/ml,未采取治疗。1年前面部开始变形,目前患者下颌明显前突,双颧隆起,鼻部内陷,双唇不能闭合(图1);牙齿松动、颅面骨质呈海绵状,同时胸廓骨骼畸形,双手杵状
患者,男,40岁,58 kg,因骨痛伴甲状旁腺激素升高19个月入院。高血压病史7年,最高达190/100 mmHg。6年前因“慢性肾功能衰竭(尿毒症期)”开始规律血液透析,2年前出现骨痛症状,19个月前发现甲状旁腺激素升高,约3 600 Pg/ml,未采取治疗。1年前面部开始变形,目前患者下颌明显前突,双颧隆起,鼻部内陷,双唇不能闭合(图1);牙齿松动、颅面骨质呈海绵状,同时胸廓骨骼畸形,双手杵状指;全身骨骼触痛明显,身高缩短10 cm。

实验室检查:甲状旁腺激素5 000pg/ml,血钙2.44 mmol/L,血磷2.14 mmol/L,血钾4.28mmol/L,碱性磷酸酶1 811 IU/L,红细胞计数2.58×1012/L,Hb 68 g/L,Hct 0.22,红细胞平均血红蛋白量26.4 pg。甲状旁腺彩超示:甲状腺右叶下部背侧深面见以实性为主的混合性回声,大小约2.5 cm×2.1 cm,形态不规则,实性部分血流较多,内并见多发条块状强回声,甲状腺左叶中部背侧见低回声,大小约1.59 cm×0.64 cm×1.26 cm,边界清。甲状腺左叶下极下方见同上性质回声,大小约1.5 cm×1.4 cm,血流较多。
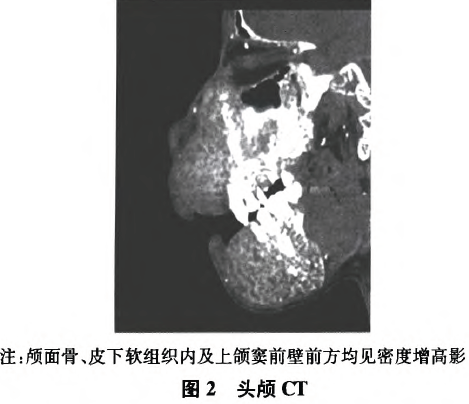
心脏彩超示:二尖瓣前叶瓣根及后叶瓣环钙化。左房增大,左室肥厚、舒张功能减低。头颅CT示:颅面骨、皮下软组织内及上颌窦前壁前方均见密度增高影(图2)。
术前评估:ASAⅢ级,MallampaiⅣ级,张口度为两横指,甲颏距离为7 cm。术前电子喉镜检查:会厌形态良好,抬举正常,舌根部淋巴滤泡增生。肾功能衰竭病史,高血压病史。心功能Ⅲ级。术前常规禁食水。患者入室后常规进行监测,BP 170/100 mmHg,HR 75次/分,SpO2 99%,建立左前臂静脉通路,局麻下行桡动脉穿刺置管,监测有创动脉血压,监测体温和BIS。患者半坐位,带牙齿护具,1%丁卡因行舌根、咽喉表面麻醉,10 min后静脉注射咪达唑仑2 mg,舒芬太尼10 ug,保留患者自主呼吸浅麻醉后,可视喉镜置入口腔,声门显露程度为Ⅱ级。撤出喉镜,静脉注射顺式阿曲库铵3 mg、丙泊酚140 mg、舒芬太尼20μg,5 min后进行气管插管入喉返神经监测气管导管,一次成功,接呼吸机行机械通气,VT 450 ml,RR 12次/分,I:E 1:2。
术中吸入七氟醚维持麻醉,七氟醚呼气末浓度1.0~1-2 MAC。术中维持BIS值40~60,BP 140 150/80~90 mmHg,HR 70~90次/分,PETCO2 35~40 mmHg。手术开始后35 min测量神经肌电信号值为1306μV,术中神经肌电信号监测顺利,术中行血气分析监测,同时通过动脉通路抽血监测甲状旁腺激素水平,围术期血气分析结果无明显变化,甲状旁腺完全切除后30 min测得甲状旁腺激素水平为334.2 pg/ml,手术历时3 h 40 min。术毕停止麻醉药吸入,8 min后BIS恢复到75,自主呼吸恢复并睁眼,握手有力,10 min后通气量恢复正常,PETCO2 35~40 mmHg,RR12~18次/分,BIS 90,意识清楚,充分吸痰后拔除气管导管,观察30 min后送返监护室。术后随访,患者无恶心、呕吐、寒战等并发症,切口VAS疼痛评分为2分,术后8 d出院。
讨论
2004年Sagliker等报道,在慢性肾功能衰竭进行透析的患者中,由于甲状旁腺功能亢进,导致患者体内钙、磷代谢紊乱,骨膜下发生一系列改变,产生的一组以面部容貌形态变化异常为主的综合征,并将其命名为Sagliker综合征。患者面部主要表现为:上颌骨向前向下整体增大,下颌骨前部垂直增大,最终导致患者的整个面容较发病前表现出明显的面部高度变大,面容似“河马”样改变。
由于Sagliker综合征患者颌面部畸形,口腔结构变化,颅面骨质呈海绵状,骨质脆,易被损伤,为可预料的困难气道。同时,神经监测下甲状腺手术要求麻醉诱导时非去极化肌松药应最小量使用,以保证术中神经肌电信号监测需要,以及慢性肾功能衰竭导致的离子紊乱、肾性贫血、高血压等伴随症状,麻醉管理难度增大。本例患者术前通过电子喉镜检查,确认患者会厌区域解剖结果无改变。根据困难气道管理指南,先行表面麻醉配合保留自主呼吸的浅麻醉方法,行可视喉镜检查,声门显露程度为Ⅱ级,为满足神经监测气管导管定位需求,给予小剂量顺式阿曲库铵,行气管插管,既保证了插管过程顺利,同时也满足术中神经监测的需求。
麻醉维持阶段采用全程吸入七氟醚,术毕患者自然苏醒,顺利完成该例患者的麻醉。Sagliker综合征为甲状旁腺功能亢进中的一种特殊病症,遵循甲状旁腺切除术的麻醉管理基础上,该类患者的术中麻醉管理应更加重视。(1)由于患者钙、磷代谢异常,术前应关注血钙水平,预防高血钙引发的心率失常。(2)该类患者常伴发骨质疏松、自发性骨折等,因此术后应轻柔搬动患者,防止发生病理性骨折。(3)该类患者颌面部畸形,气管插管可能困难,牙齿松动,与上颌连接不牢固,应使用保护牙齿的器具。(4)此类患者均伴慢性肾功能衰竭,因此,应用麻醉药物原则为尽可能减少肾功能损害。唐之音等研究表明,应用以上药物后均未发生苏醒延迟、呼吸抑制等并发症。(5)如声门显露程度为工或Ⅱ级,可采用咽喉部表面麻醉加保留自主呼吸浅麻醉的方法,先行可视喉镜检查,了解声门暴露情况后,采用1倍ED95顺式阿曲库铵配合常规剂量丙泊酚、舒芬太尼诱导,既保证插管过程顺利,也保证了术中神经肌电信号监测的需求。如声门显露程度为Ⅲ或Ⅳ级,可采用纤维支气管镜下插入加强型气管插管,这与Papadima等推荐的方法一致,术中甲状腺科医师需插入针状电极完成神经肌电信号监测。
原始出处:
李琳琳,张春璐,陈鹏.Sagliker综合征患者甲状旁腺切除术麻醉一例[J].临床麻醉学杂志,2018,34(12):1239-1240.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Sagliker综合征#
29
#切除术#
28
#综合征#
32
#甲状旁腺#
35
#甲状旁腺切除术#
50