EUR J Cancer: buparlisib联合拉帕替尼治疗曲妥珠单抗拮抗的HER2阳性晚期乳腺癌
2017-12-24 MedSci MedSci原创
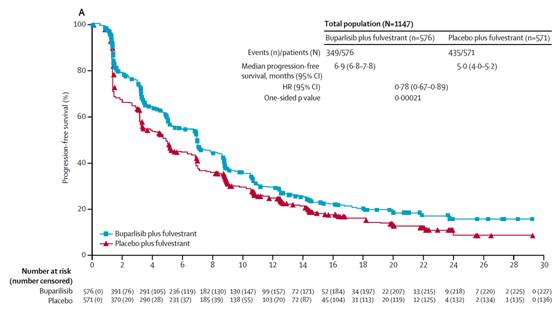
磷脂酰肌醇3-激酶(PI3K)/ AKT /mTOR通路在HER2阳性乳腺癌细胞中经常被激活并且可能在曲妥珠单抗拮抗中发挥重要作用。 Buparlisib是强效的泛PI3K抑制剂,对野生型和突变型PI3K p110均具有抑制作用。因此buparlisib理论上能够治疗曲妥珠单抗耐受的HER2阳性晚期乳腺癌患者。 在一项以确定最大耐受剂量(maximum tolerated dose,MTD)
磷脂酰肌醇3-激酶(PI3K)/ AKT /mTOR通路在HER2阳性乳腺癌细胞中经常被激活并且可能在曲妥珠单抗拮抗中发挥重要作用。 Buparlisib是强效的泛PI3K抑制剂,对野生型和突变型PI3K p110均具有抑制作用。因此buparlisib理论上能够治疗曲妥珠单抗耐受的HER2阳性晚期乳腺癌患者。
在一项以确定最大耐受剂量(maximum tolerated dose,MTD)的I期临床试验中,患者每日口服buparlisib(40,60或80mg)和拉帕替尼(750,1000或1250mg),疗程结束后对药物的抗肿瘤活性和药代动力学(PK)进行评估。在入组的24名患者中,药物相关的主要不良反应事件包括腹泻,恶心,皮疹,虚弱,抑郁,焦虑和转氨酶增加,没有明显的药物与药物之间相互作用的药代动力学证明。值得注意的是,治疗组中癌症的控制率高达79%[95%置信区间57-92%],且1例患者完全缓解。
因此,通过疾病的控制率发现,buparlisib联合拉帕替尼治疗曲妥珠单抗拮抗的HER2阳性晚期乳腺癌的方案是可行的。
原始出处:
Guerin, Mathilde, et
al. "PIKHER2: A phase IB study evaluating buparlisib in combination with
lapatinib in trastuzumab-resistant HER2-positive advanced breast cancer."
European Journal of Cancer 2017 86: 28-36. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曲妥珠#
46
#buparlisib#
37
#uPAR#
50
#HER2阳性晚期乳腺癌#
57
#HER2阳性#
31
#拉帕替尼#
27