Lancet子刊:肺炎球菌可把这个动脉瘤玩大了——案例报道
2016-11-13 MedSci MedSci原创
77岁女性,发热、意识状态改变、颈部僵硬。她是个烟鬼,有高血压和血脂异常,3天前有右侧背部疼痛。 头部CT和胸片均正常,腰椎穿刺和血培养显示肺炎球菌性脑膜炎和菌血症。 开始头孢曲松治疗(2 g,每日2次),患者病情迅速好转,发热解决了,炎症标志物也大量减少了(白细胞计数从19·7/ml下降到14·9/ml,C反应蛋白由225 mg/L下降到108 mg/L)。 然而,病人入院后1
77岁女性,发热、意识状态改变、颈部僵硬。她是个烟鬼,有高血压和血脂异常,3天前有右侧背部疼痛。
头部CT和胸片均正常,腰椎穿刺和血培养显示肺炎球菌性脑膜炎和菌血症。
开始头孢曲松治疗(2 g,每日2次),患者病情迅速好转,发热解决了,炎症标志物也大量减少了(白细胞计数从19·7/ml下降到14·9/ml,C反应蛋白由225 mg/L下降到108 mg/L)。
然而,病人入院后12天,临床和生化改善不到一周,她的背痛情况出现恶化,炎症标志物反弹(白细胞计数19·8/ml,C-反应蛋白为171 mg/L)。
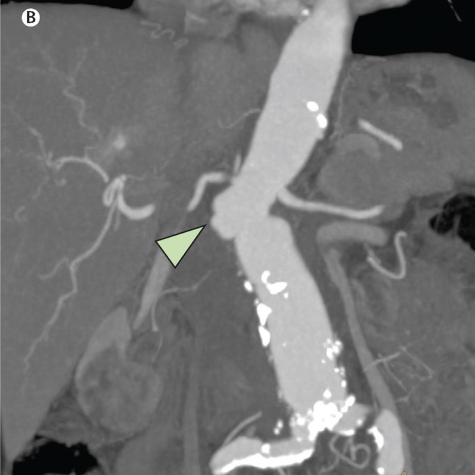
腰椎CT没有发现感染,但有腹主动脉增大,有动脉瘤周围炎症的迹象。CT血管造影检查证实了腹主动脉瘤的存在,并有即将破裂的迹象。

真菌性动脉瘤和微生物血管炎是罕见的,通常发生在有潜在动脉粥样硬化血管疾病的患者中,是菌血症播种异常主动脉表面的后果。临床表现往往是亚急性的,诊断往往延迟或作不出诊断,直到死亡后。尽管肺炎链球菌是菌血症的常见原因,却很少引起血管播种。肺炎球菌主动脉炎应排除有典型腹主动脉瘤症状、高危心血管疾病的脓毒症患者。
病人及时进行了同种主动脉-主动脉瓣置换术。术后患者恢复可,没有任何并发症。然而,1个月后的CT血管造影显示,疾病似乎又开始进展了。
但病人拒绝任何手术。从那时起,对患者进行严格的临床和放射学随访检查,不够没有发现并且进一步恶化的证据。经过近12个月,她仍然活着,临床情况也较好。
原始出处:
Davide Mangioni,et al.Abdominal aortitis and aneurysm impending rupture during pneumococcal meningitis.The Lancet Infectious Diseases.Volume 16, No. 8, p980, August 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
28
了解了解!
67
#肺炎球菌#
44
很好,不错,以后会多学习
67
学习新知识谢谢分享。
70
学习了,赞一个!
60
看看,学习一下
62