Br J Cancer:新辅助伊马替尼在胃肠间质瘤中的II期研究
2017-07-16 豆芽菜 艾兰博曼医学网
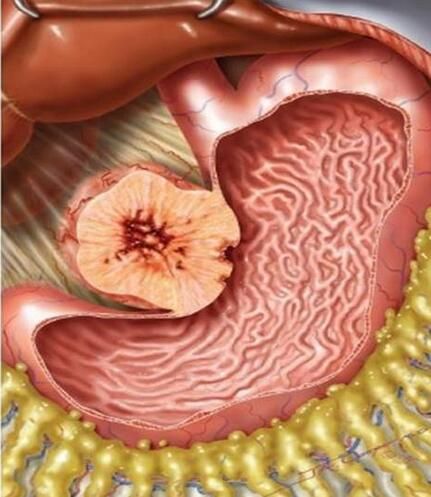
胃肠道间质瘤(GIST)是胃肠道中最常见的间充质肿瘤,大部分源于胃。手术切除是GIST唯一的治疗方法。 切除后复发的独立预后因素包括肿瘤大小,有丝分裂计数,肿瘤位置和肿瘤破裂。具有肿瘤大小,高有丝分裂细胞数,肿瘤破裂等高风险特征的GIST在切除后预后差。一半以上的这种肿瘤患者在手术后5年内发生复发。对于这种高风险肿瘤,尽力用辅助治疗以降低复发率。即使给予辅助治疗胃肠道间质瘤(GIST)患病风险依然
胃肠道间质瘤(GIST)是胃肠道中最常见的间充质肿瘤,大部分源于胃。手术切除是GIST唯一的治疗方法。 切除后复发的独立预后因素包括肿瘤大小,有丝分裂计数,肿瘤位置和肿瘤破裂。具有肿瘤大小,高有丝分裂细胞数,肿瘤破裂等高风险特征的GIST在切除后预后差。一半以上的这种肿瘤患者在手术后5年内发生复发。对于这种高风险肿瘤,尽力用辅助治疗以降低复发率。即使给予辅助治疗胃肠道间质瘤(GIST)患病风险依然较高而且预后较差。 新辅助伊马替尼可能通过收缩大GIST并维持器官功能来提高治愈率。
近日,大阪大学医学院胃肠外科研究者在British Journal of Cancer杂志发表了“Phase II study of neoadjuvant imatinib in large gastrointestinal stromal tumours of the stomach”的研究,本研究对胃GIST≥10cm的患者进行了亚洲多国II期研究。患者接受新辅助伊马替尼(400 mg /天),治疗6-9个月。 主要终点为R0切除率。
研究共计56例患者。对53例患者进行全面分析,46例患者完成了≥6个月的新辅助伊马替尼。 3-4级中性粒细胞减少症和皮疹发生率分别为8%和9%,但没有治疗相关的死亡。RECIST的反应率为62%(95%CI,48-75%)。R0切除率为91%(48/53)(95%CI,79-97%)。在48例R0切除术患者中,42例中保存了至少一半的胃。在32个月的中位随访时间,2年总体和无进展生存率分别为98%和89%。
研究表明,6-9个月的新辅助伊马替尼治疗有望成为大型胃GIST的有效疗法,并在可接受的毒性范围内允许高R0切除率。
原始出处:
Yukinori Kurokawa, Han-Kwang Yang, et al. Phase II study of neoadjuvant imatinib in large gastrointestinal stromal tumours of the stomach. British Journal of Cancer (2017) 117, 25–32. doi:10.1038/bjc.2017.144 www.bjcancer.com
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新辅助#
36
很好,不错,以后会多学习
66
很好,不错,以后会多学习
0
现在的观点倾向于终身服用伊马替尼直至无效
52
#间质瘤#
42
学习了,谢谢分享
67
学习了学习了学习了
0
很好,不错,以后会多学习
22