Nat Commun:中国科大等在炎症发生机制研究方面取得进展
2017-08-09 佚名 中国科技大学
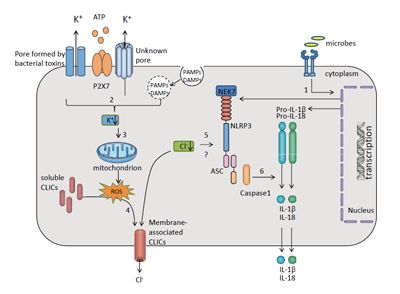
<div style="text-align: left;"><span>近日,中国科学技术大学生命科学学院、微尺度国家实验室(筹)、医学中心及中国科学院天然<a class="channel_keylink" href="http://www.medsci.cn/guideline/list.do?q=%E5%85%8D%E7%96%AB" target="_blank">免疫</a>和慢性疾病重点实验室教授周荣斌、江维研究组与王均研究组、白丽研究组及中山大学教授崔隽研究组合作,揭示了胞内氯离子通道蛋白CLICs家族在NLRP3炎症小体活化中的重要作用。该项研究成果于8月4日发表在《自然-通讯》杂志。</span></div><div><br></div><div>炎症反应是机体一种重要的<a class="channel_keylink" href="http://www.medsci.cn/guideline/list.do?q=%E5%85%8D%E7%96%AB" target="_blank">免疫</a>防御机制,有助于机体抵抗病原微生物<a class="channel
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#国科大#
39
#机制研究#
30
#COMMUN#
36
#Nat#
30
#发生机制#
24
学习了,涨姿势
40