围术期疼痛的全程管理病例_老年患者行右半结肠癌根治术围术期镇痛管理病例
2017-10-26 CMT 中国医学论坛报
患者男性,80岁,体重50 kg,身高175 cm。因“反复腹痛、腹胀、腹泻伴恶心呕吐1月”入院,术前诊断“右半结肠占位性病变并肠梗阻”,拟行“右半结肠癌根治术”,患者自发病以来,食欲欠佳,精神较差,睡眠较差,体重减轻5 kg。
病例摘要
患者男性,80岁,体重50 kg,身高175 cm。因“反复腹痛、腹胀、腹泻伴恶心呕吐1月”入院,术前诊断“右半结肠占位性病变并肠梗阻”,拟行“右半结肠癌根治术”,患者自发病以来,食欲欠佳,精神较差,睡眠较差,体重减轻5 kg。
患者既往有高血压病史13 年,最高190/100 mmHg,目前口服硝苯地平30 mg qd,血压控制平稳;且存在冠心病病史,半年前行“不停跳冠脉搭桥术”(左前降支、回旋支、右冠三支),目前服用氯吡格雷和阿托伐他汀钙。患者行冠脉搭桥术后发生严重认知功能障碍,表现为记忆力下降,意识混乱,目前恢复良好。近期夜间经常有胸闷、胸痛。前列腺增生病史多年,无糖尿病、脑血管病史。
辅助检查
心脏超声示“右心及左房大,左室壁运动不协调,升主动脉扩张,主动脉瓣及二尖瓣退行性变伴钙化,二、三尖瓣中度反流,主动脉瓣轻-中度反流”,动脉血气氧分压(PO2)73.4 mmHg,脑钠肽(BNP)1466 pg/ml,总蛋白51.5 g/L,白蛋白31.5 g/L。患者美国麻醉医师协会(ASA)分级Ⅳ级。因患者目前合并有完全性机械性肠梗阻,需要行急诊手术,无法进一步评估心脏功能。
麻醉情况
患者入室后常规监护生命体征,脑电双频指数(BIS)监测麻醉深度。羟考酮2 mg(生理盐水稀释至1 mg/ml)静脉注射,局麻下行颈内静脉穿刺和桡动脉测压。以羟考酮8 mg、丙泊酚40 mg、顺式阿曲库铵16 mg行麻醉诱导。诱导成功后于超声引导下0.33%罗哌卡因两侧各15 ml 行腹直肌后鞘神经阻滞。术中予以丙泊酚、瑞芬太尼、七氟醚静吸复合维持麻醉,根据手术刺激强度和BIS值调整镇静、镇痛药剂量,需要时予以小剂量去甲肾上腺素间断泵注维持循环稳定。手术时间3 h,手术结束前30 min静脉推注羟考酮3 mg。术毕10 min 左右患者意识恢复,自主呼吸恢复,潮气量300 ml,呼吸频率14次/min,顺利拔除气管导管,患者无明显不适,应答准确,连接静脉自控镇痛(PCIA),返回病房。术后静脉泵注右美托咪定0.05 μg/(kg·h)直至次日晨8时。
PCIA 配方为羟考酮50 mg 以生理盐水稀释至100 ml。无首次剂量,背景剂量2 ml/h,单次剂量4 ml,锁定时间10 min。
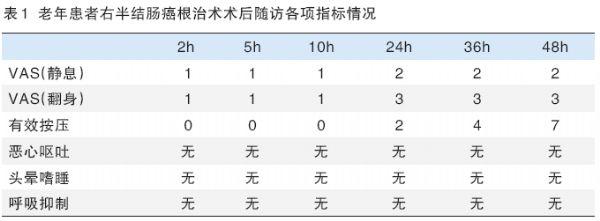
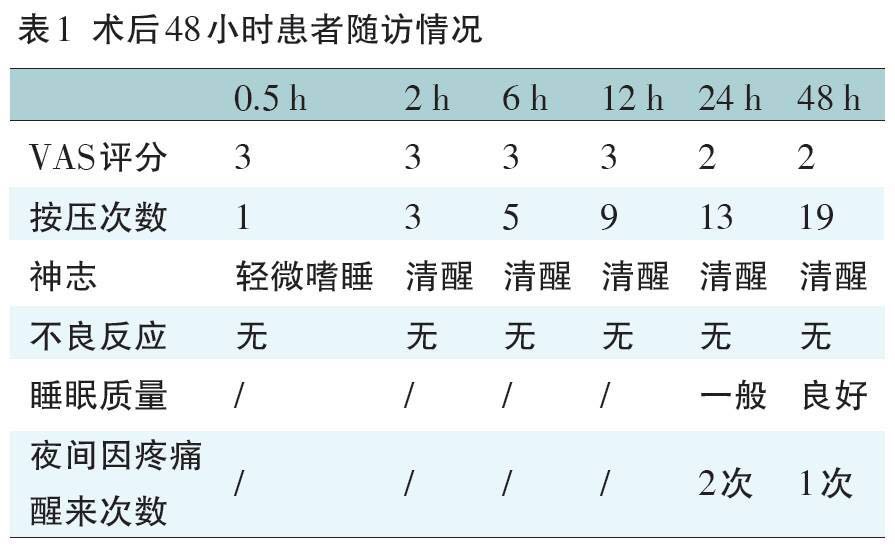
患者术后处于安静合作状态,镇痛效果及舒适度良好,对镇痛效果满意。Ramsay镇静评分和视觉模拟(VAS)评分如表1。患者术后无呼吸抑制、头晕嗜睡等不良反应。术后48 h有效按压次数7次,总按压次数7次。
老年患者常合并有各种内科疾病,此例患者合并有高血压、冠心病,目前心绞痛经常发作,提示冠心病控制不佳。去年冠脉搭桥术后患者有严重的认知功能障碍,表现为记忆力下降,意识混乱,家属对此非常担心。但在完全性肠梗阻的急症情况下,没有过多的时间完善检查和控制病情,因此只能在最小的干扰下完成手术,术中术后采取合适的镇痛方式控制应激状态。
羟考酮是阿片μ、κ双受体激动剂,对内脏痛和躯体痛均有较好的镇痛效果,与其他镇痛药物如舒芬太尼、曲马多、非甾体类药相比,在治疗内脏痛方面有独特的优势。羟考酮起效快,2~3 min起效,作用强度大,应用于麻醉诱导,抑制气管插管应激效果好,安全范围广;持续镇痛时间长达4 h,既能很好地用于围术期镇痛,又能避免频繁用药导致的副作用;作为水溶性药物,脂溶性低,不易蓄积,代谢产物无临床镇痛作用,可安全应用于高龄患者。
此外,针对本例患者我们还采用了综合措施改善其预后,如使用腹壁神经阻滞的方式复合镇痛,采用BIS监测精准控制麻醉深度,术后泵注小剂量右美托咪定改善手术日当晚睡眠,手术后医护人员和家属多关心其心理状态,帮助患者安全舒适地渡过了围术期。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#管理病例#
33
#围术期#
44
#镇痛#
45
#根治术#
29
#全程管理#
40
#根治#
28
学习了受益匪浅
65