NEJM:美托洛尔预防COPD急性加重的疗效分析
2019-12-12 xing.T MedSci原创
由此可见,在中度或重度COPD患者中,尚未确定使用β-受体阻滞剂的指征,美托洛尔组和安慰剂组出现首次COPD恶化的时间相似。在接受美托洛尔治疗的患者中,因加重而住院治疗更为常见。
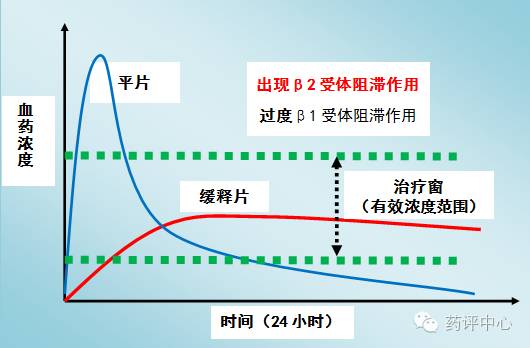
观察性研究表明,β受体阻滞剂可以降低中度或重度慢性阻塞性肺疾病(COPD)患者加重和死亡的风险,但这些发现尚未在随机试验中得到证实。近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项前瞻性随机试验中,研究人员将40至85岁年龄段的COPD患者随机分配接受β受体阻滞剂(美托洛尔缓释剂)或安慰剂治疗。所有患者都有COPD的临床病史,伴有中度气流受限和增加的加重风险,以一年前加病史或按规定吸氧来明确。研究人员排除了已经服用β受体阻滞剂或已明确使用此类药物的患者。该研究的主要终点是治疗期间直至COPD首次加重的时间,范围为336至350天,具体取决于美托洛尔的调整剂量。该研究共有532名患者接受了随机分组。患者的平均(±SD)年龄为65.0±7.8岁;1秒内用力呼气量(FEV1)平均值为预测值的41.1±16.3%。由于对主要终点和安全方面的考虑,该试验提前终止。组间首次发作前的中位时间无显著差异,美托洛尔组为202天,安慰剂组为222天(美托洛尔与安慰剂的风险比为1.05;95%置信区间[CI]为0.84至1.32;P=0.66)。美托洛尔与加重导致住院的风险更高(风险比为1.91;95
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#急性加重#
44
#疗效分析#
35
#美托洛尔#
37
谢谢梅斯提供这么好的信息,学到很多
74
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
71