JAMA:TAVR后感染性心内膜炎的危险因素及临床疗效分析
2016-09-14 MedSci MedSci原创
根据9月13日发表在JAMA的一项研究,接受经导管主动脉瓣置换术,年轻,男性,有糖尿病史,以及中度至重度残余主动脉瓣关闭不全的患者患感染性心内膜炎的风险显著增加,患心内膜炎的患者有较高的住院死亡率高和2年死亡率。1%至6%的患者在接受外科瓣膜置换术后感染性心内膜炎(由于细菌进入血液引起的感染,这些细菌会隐藏在心脏瓣膜或心内膜中),这增加了疾病和死亡的风险。经导管主动脉瓣置换术(TAVR)已成为主动
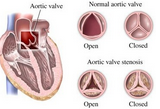
根据9月13日发表在JAMA的一项研究,接受经导管主动脉瓣置换术,年轻,男性,有糖尿病史,以及中度至重度残余主动脉瓣关闭不全的患者患感染性心内膜炎的风险显著增加,患心内膜炎的患者有较高的住院死亡率高和2年死亡率。1%至6%的患者在接受外科瓣膜置换术后感染性心内膜炎(由于细菌进入血液引起的感染,这些细菌会隐藏在心脏瓣膜或心内膜中),这增加了疾病和死亡的风险。经导管主动脉瓣置换术(TAVR)已成为主动脉瓣狭窄患者的治疗选择,但其也被认为具有很高的手术风险性。目前关于TAVR后感染性心内膜炎的患者临床特点及患者的预后数据非常有限。加拿大拉瓦尔大学心肺研究所的医学博士Josep Rodes-Cabau和同事分析了TAVR国际登记后患感染性心内膜炎的数据,其中包括TAVR后明确感染性心内膜炎的患者,这些患者来自欧洲、北美和南美的47个中心,该研究包括了从2005年6月到2015年10月的数据。在接受TAVR的20006例患者中,共有250例患者患感染性心内膜炎(发病率为每人年1.1%;平均年龄80岁;64%为男性)。从TAVR到感染性心内膜炎的平均时间为5.3个月。TAVR后患感染性心内膜炎的高
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#内膜#
44
#AVR#
44
#感染性#
36
#疗效分析#
35
#临床疗效#
51
很好的内容,谢谢分享。
68
很好的内容,谢谢分享。
72
#心内膜炎#
39