Cell Mol Biol (Noisy-le-grand):中国过敏性鼻炎儿童IL-31, IL-33和ST2血清水平调查
2018-10-21 AlexYang MedSci原创
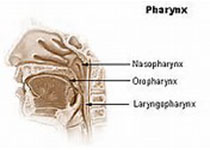
最近,有研究人员比较了儿童过敏性鼻炎(AR)和过敏性哮喘患者中IL-31, IL-33和ST2血清水平,并尝试阐释AR的发病机制。研究包括了36名患有间歇性AR的儿童患者,调查的时间为2013年1月到2016年12月。研究人员设置了2个对照组,过敏性哮喘组和健康对照组,并对所有参与者的过敏状态通过皮刺测试(SPT)进行了测试和确定,还利用ELISA对IL-31, IL-33和ST2血清水平进行了确
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
41
#过敏性#
31
#血清水平#
50
#CEL#
39
#ST2#
36
#Biol#
29
#Bio#
35
#Grand#
37
#IL-33#
46
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
70