BMJ:50岁之前都来得及!分析25年数据发现,50岁时的生活习惯和心血管健康评分每多1分,与痴呆风险降低11%相关
2019-08-12 奇点糕 奇点网
老年痴呆可以说是最让人绝望的一种病了,看着自己的亲人一点点糊涂下去却又束手无策的感觉,想必十分不好受。在老年痴呆的一大原因——AD的发生发展中,脑血管的收缩和脑血流量的下降有着十分重要的意义。毕竟作为能耗最高的器官,没有充足的血供可不行。而保证大脑充足的血供,除了脑血管的畅通,一颗健康的心脏也是必不可少的。近日,巴黎大学的Séverine Sabia和Archana Singh-Manoux等
老年痴呆可以说是最让人绝望的一种病了,看着自己的亲人一点点糊涂下去却又束手无策的感觉,想必十分不好受。
在老年痴呆的一大原因——AD的发生发展中,脑血管的收缩和脑血流量的下降有着十分重要的意义。毕竟作为能耗最高的器官,没有充足的血供可不行。而保证大脑充足的血供,除了脑血管的畅通,一颗健康的心脏也是必不可少的。
近日,巴黎大学的Séverine Sabia和Archana Singh-Manoux等对7899人近25的随访研究发现,用来评估心血管健康的Life’s Simple 7评分,也与25年内的痴呆风险有关。7项评分的总和每多1分,痴呆风险降低11%。相关研究发表在BMJ上[1]。
左一为Archana Singh-Manoux
(来自fondationbs.org)
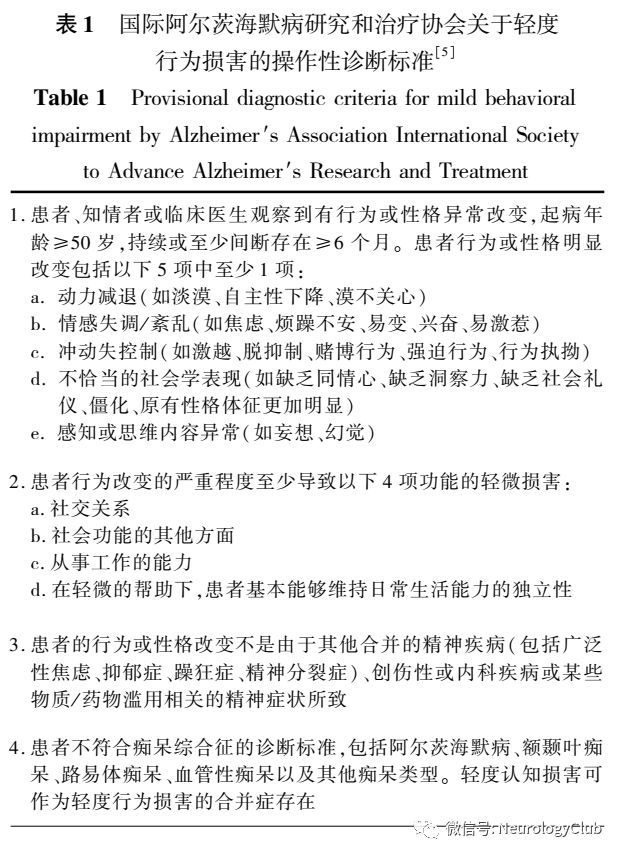
AD等等的老年痴呆症,发病过程可以说是十分漫长,在出现临床表现前15~20年,常常就已经有了一些病理改变[2]。漫长的病程让AD的药物研发十分困难,各大制药公司纷纷弃坑,但反过来说的话,这样漫长的病程,也让我们有了充足的时间来对痴呆症进行预防。
至于怎么预防,美国和欧洲的指南都建议,把目标对准中年时的心血管风险因素。
人到中年,往往正处在事业的巅峰期,各种应酬不断,大鱼大肉抽烟喝酒更是家常便饭,锻炼更是没有时间,身上肥肉越来越多,高血压高血脂高血糖的三高也少不了。这些可都是心血管疾病的危险因素。
中年是发福的年纪
(来自pixabay.com)
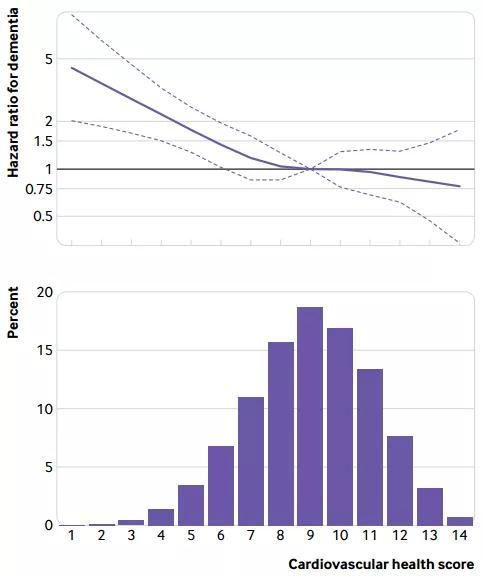
根据这些危险因素,美国心脏协会(AHA)提出了Life’s Simple 7评分,通过吸烟、饮食、锻炼这三项日常活动,以及BMI、血压、空腹血糖、血胆固醇这四项生理指标(详细评分标准见后文),简单的评估一个人的心血管健康[3]。评分较高的人,患2型糖尿病,以及冠心病、中风等心血管疾病的风险都要更低[4,5]。
心血管系统遍布全身各处,人体组织获取营养、排出废物,乃至一些信号的传递,都要靠心血管系统来实现,大脑当然也不例外。此前就有研究显示,老年人中较高的心血管健康评分,与认知衰退的减缓和痴呆风险的降低有关[6]。
或许,心血管风险和痴呆之间的关系,在中年时就开始了。研究人员使用Whitehall II队列中1万余人将近30年的数据进行了研究。
Whitehall是伦敦一条有许多政府部门的街道,Whitehall II研究中的参与者都是英国公务员
(来自wikimedia.org)
研究人员提取了队列中每个参与者50岁时,Life’s Simple 7评分涉及的7项指标的数据,按不佳、中等、优良分别给0、1、2分。同时,研究人员从电子健康记录中获取了参与者们的死亡和痴呆情况。
最终,7899名数据完整的参与者被纳入了研究。他们基线时平均年龄50.4岁,67.6%为男性。在中位24.7年的随访中,有347人被诊断为痴呆,平均诊断年龄为75.3岁。
Life’s Simple 7评分标准
研究人员发现,心血管疾病确实与痴呆有着密切关系。患有心血管疾病与痴呆风险增加96%相关。
而在心血管健康不佳,Life’s Simple 7总分0~6分的参与者中,平均每1000人年要诊断3.2例痴呆。而总分7~11分和总分12~14分的参与者中,每1000人年分别只有1.7例和1.3例痴呆,痴呆风险分别比0~6分的人低了39%和43%。
经进一步统计,研究人员发现,Life’s Simple 7总分每多1分,痴呆风险降低11%!即使在排除了已经发生的心血管疾病的影响后,每多1分的痴呆风险也会降低9%!
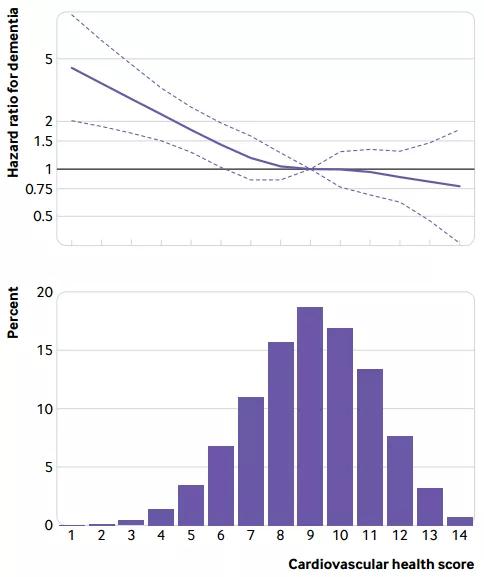
不同Life’s Simple 7评分的参与者比例(下),以及他们的相对痴呆风险(上)
而且50岁时的Life’s Simple 7评分只与患心血管疾病前的痴呆风险有关,每多1分与痴呆风险降低11%相关。但如果已经患了心血管疾病,痴呆风险就与50岁时的评分无关了。
心血管健康和痴呆之间的关系不一定需要有临床表现的心血管疾病!种种心血管风险因素可能能直接增加痴呆风险!
此外,脑容量也与Life’s Simple 7评分有关。研究人员对708名平均69.9岁时有MRI数据的参与者分析发现,心血管评分每多1分,与全脑体积增加0.14%,灰质体积增加0.12%相关,大约相当于年轻了5~6个月。
研究人员表示:“心血管风险因素是可以改变的,这使得它们成为重要的战略预防目标。这项研究支持旨在改善50岁心血管健康的公共卫生政策,以促进认知健康。”
参考文献:
1. Sabia S, Fayosse A, Dumurgier J, et al. Association of ideal cardiovascular health at age 50 with incidence of dementia: A 25-year follow-up study[J]. British Medical Journal, 2019.
2. Jack Jr C R, Knopman D S, Jagust W J, et al. Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers[J]. The Lancet Neurology, 2013, 12(2): 207-216.
3. Lloyd-Jones D M. American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goats for cardiovascular health promotion and disease reduction: the American Heart Association's Strategic Impact Goal through 2020 and beyond[J]. Circulation, 2010, 121: 586-613.
4. Joseph J J, Echouffo-Tcheugui J B, Carnethon M R, et al. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis[J]. Diabetologia, 2016, 59(9): 1893-1903.
5. Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: a meta-analysis[J]. International journal of cardiology, 2016, 214: 279-283.
6. Samieri C, Perier M C, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia[J]. Jama, 2018, 320(7): 657-664.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#生活习惯#
44
#BMJ#
0
#风险降低#
26
#痴呆风险#
25
老年人痴呆何药可用??
50