JCEM:IPSS可提高库欣病诊断的准确性
2013-04-09 JCEM 丁香园
CRH刺激后的不同反应类型 在术前MRI正常的库欣病(CD)患者往往很难找到一个腺瘤。需要更好的定位方式。为了确定岩下窦取样(IPSS)预测单侧腺瘤的准确性,来自美国弗吉尼亚大学健康科学中心神经外科的Edward H Oldfield博士及其团队进行了一项研究,该研究发现IPSS可以提高库欣病的诊断的准确性。该研究结果在线发表在2012年4月3日的美国《临床内分泌代谢杂志》(The journa
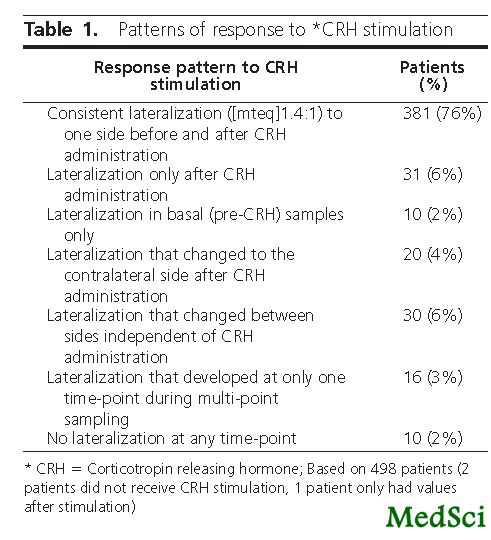
CRH刺激后的不同反应类型
在术前MRI正常的库欣病(CD)患者往往很难找到一个腺瘤。需要更好的定位方式。为了确定岩下窦取样(IPSS)预测单侧腺瘤的准确性,来自美国弗吉尼亚大学健康科学中心神经外科的Edward H Oldfield博士及其团队进行了一项研究,该研究发现IPSS可以提高库欣病的诊断的准确性。该研究结果在线发表在2012年4月3日的美国《临床内分泌代谢杂志》(The journal of clinical endocrinology & metabolism)上。
该研究是一项在三级医疗临床研究中心进行的前瞻性观察性研究,包括501例确诊ACTH腺瘤和IPSS的患者(女性363例)。主要研究结果是IPSS预测蝶鞍内腺瘤偏侧优势的准确性。
该研究结果表明,IPSS证实了491例患者(98%)的ACTH分泌为垂体来源的。共有10例患者有假阴性结果,峰值IPSS ACTH浓度<400pg/ml(促肾上腺皮质激素释放激素(CRH)刺激前后)。在491例患者(98%)两侧下岩窦ACTH的比值为1.4。这个比值在273/396例(PPV=69%)伴有一侧腺瘤的患者中准确预测偏侧优势。左侧IPSS偏侧优势(P=0.008)和CRH治疗前后的偏侧优势一致(P=0.02)与准确性的增高相关。在171/201例(PPV=86%)患者积极的术前MRI与肿瘤位置有关。
该研究发现,IPSS在库欣病的鉴别诊断中,最常见的诊断错误类型是潜在的假阴性结果,可以由峰值IPSS ACTH值<400pg/ml鉴别。当MRI正常时,IPSS可以用于在术前影像学阴性的患者引导手术探查。然而,由于偏侧优势的准确度有限,当依据预测位置腺瘤不易发现时,脑垂体彻底探查是需要的。
与库欣病相关的拓展阅读:
- FDA批准帕瑞肽治疗库欣病 更多信息请点击:有关库欣病更多资讯

The lateralization accuracy of inferior petrosal sinus sampling
Abstract
Context.It is often difficult to find an adenoma in patients with Cushing's disease (CD) whose preoperative MRI is normal. Better localizing modalities are needed.Objective.To determine the accuracy of inferior petrosal sinus sampling (IPSS) to predict adenoma lateralization.Design.Prospective observational studySetting.A tertiary care clinical research centerPatients.501 consecutive patients (363 female) with confirmed ACTH adenomas and IPSS were included.Intervention.IPSSMain outcome measure.Accuracy of IPSS to predict the intra-sellar location of an adenoma.Results.IPSS confirmed a pituitary source of ACTH secretion in 491 patients (98%). All 10 patients with false negative results had peak IPSS ACTH concentrations (before or after corticotropin releasing hormone, CRH) of <400pg/ml. Interpetrosal (side-to-side) ratios were [mteq]1.4 in 491 patients (98%). This ratio correctly predicted lateralization in 273/396 patients (PPV = 69%) with a lateral adenoma. Left-sided IPSS lateralization (p =0.008) and consistent lateralization before and after CRH administration (p=0.02) were associated with enhanced accuracy. When positive, preoperative MRI correlated with adenoma location in 171/201 patients (PPV = 86%).Conclusions.Potential false negative results, the most common type of diagnostic error with IPSS for the differential diagnosis of CS, can be identified by peak IPSS ACTH values < 400 pg/ml. When MRI is normal, IPSS can be used to guide surgical exploration in patients with negative preoperative imaging. However, because of the limited accuracy of lateralization, thorough exploration of the pituitary gland is required when an adenoma is not readily discovered based on predicted location.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#准确性#
26
#JCEM#
30
#JCE#
34
#iPS#
43
#库欣病#
33