盘点:结直肠癌研究进展一览
2017-08-24 MedSci MedSci原创
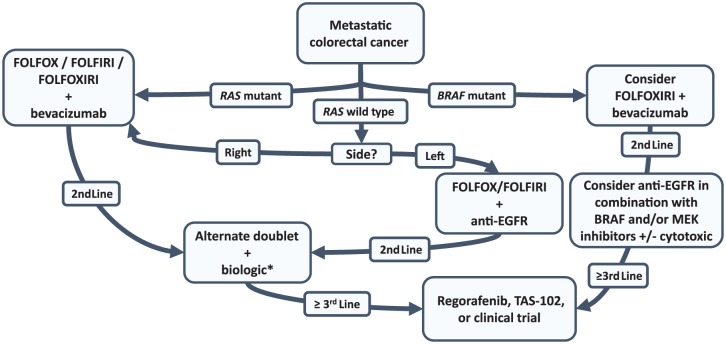
结直肠癌是我国最为常见的癌症之一,近年来发病率呈不断上升的趋势,尤其在一些地区年龄超过50岁的人,更是肠癌的多发人群,不论男女,结肠癌与直肠癌的发病比例约各占其半。而且城市远高于农村,多数患者发现时已属于中晚期。梅斯医学小编整理了关于结直肠癌的最新研究进展,与大家分享! 【1】Lancet Oncol:TAS-102+贝伐单抗可用于治疗难治性的转移性结直肠癌 http://www.
结直肠癌是我国最为常见的癌症之一,近年来发病率呈不断上升的趋势,尤其在一些地区年龄超过50岁的人,更是肠癌的多发人群,不论男女,结肠癌与直肠癌的发病比例约各占其半。而且城市远高于农村,多数患者发现时已属于中晚期。梅斯医学小编整理了关于结直肠癌的最新研究进展,与大家分享!
【1】Lancet Oncol:TAS-102+贝伐单抗可用于治疗难治性的转移性结直肠癌
尿苷和盐酸盐复方药物具有显着的总体生存效益。在临床前模型中,TAS-102+贝伐单抗,与单独使用二者任何一个药物相比,其在对抗结肠直肠癌异种移植的活性中表现出了增强。近日,在医学杂志Lancet Oncol上面发表了一篇研究文章,该文章旨在评估TAS-102+贝伐单抗的活性和安全性。
研究显示:2014年2月25日至2014年7月23日,研究人员招募了25名转移性结肠直肠癌患者:第1期6例,第2期19例患者。在第1期接受TAS-102的6名患者没有剂量限制性毒性,这被认为是RP2D。在接受RP2D的21例患者中,9例没有进行集中评估事件进展;16周无进展生存率为42.9%(80% CI 27.8-59.0)。在所有25例患者中,最常见的3级或更严重的不良事件是中性粒细胞减少症(18例[72%]患者),白细胞减少(11%[44%]),贫血(4[16%]),发热性中性粒细胞减少(4[16%]),血小板减少症(3例[12%])。三例(12%)患者报告了与治疗相关的严重不良事件。此研究没有发生治疗相关的死亡事件。
由此可见,TAS-102+贝伐单抗具有治疗安全性及活性,可能成为难治性的转移性结肠直肠癌患者的潜在治疗选择。
【2】Nutrition:警示!“炎症性饮食”或增加结直肠癌风险
慢性炎症可造成癌症。饮食通过改变炎症生物标志物的循环水平而在调节慢性炎症中起到重要作用。2017年6月,发表在《Nutrition》的一项在加拿大纽芬兰进行的基于人群的病例对照研究调查了炎症性饮食和结直肠癌风险之间的相关性。慢性炎症可造成癌症。饮食通过改变炎症生物标志物的循环水平而在调节慢性炎症中起到重要作用。单一食物或营养素对癌症的影响尚不确定。本研究旨在确定饮食的促炎症潜力与结直肠癌(CRC)风险之间的相关性。
总共纳入了547例CRC病例(来自于纽芬兰结直肠癌注册)和686例来自于普通人群的对照。社会人口学、用药史、生活方式和169条目的食物频率调查问卷等数据从两组中回顾性收集。研究者计算了饮食炎症指数(DII)评分,并用作分类和连续变量进行分析。调整了潜在混杂因素后的多变量逻辑回归用于评估比值比。使用每个四分位数的中位值进行趋势的线性检验。
调整后总能量的平均DII评分为-0.81(范围:-5.19~6.93)。病例(-0.73±1.5)比对照(-0.89±1.6)的DII评分稍高(P=0.04)。调整潜在混杂因素后,无论使用DII作为连续变量(OR,1.10;95% CI,1.01~1.20),还是作为分类变量(OR,1.65;95% CI,1.13~2.42),DII评分和CRC风险之间均具有统计学显着的相关性(P=0.02)。
结果表明,纽芬兰人群中,促炎症饮食与CRC风险的增加相关。
【3】ANN SURG:Ⅱ/Ⅲ期低位直肠癌系膜切除术是否需要进行侧方淋巴结清扫
Ⅱ期或Ⅲ期低位直肠癌有时会出现盆腔侧方淋巴结转移。在日本,直肠系膜切除术(ME)联合侧方淋巴结清扫(LLND)是标准治疗方式,而国际上直肠癌的标准外科治疗方式仅为直肠系膜切除术。ANN SURG近期发表了一篇文章,研究直肠系膜切除术是否劣效于直肠系膜切除术联合侧方淋巴结清扫。
研究的纳入标准主要有病理确诊为直肠癌且临床分期为Ⅱ/Ⅲ期,主要位于直肠,肿瘤下缘在腹膜反折以下,盆腔侧方淋巴结无肿大,年龄20-75岁。患者在手术时随机分为ME联合LLND组或ME组。研究主要终点是无复发生存,次要终点包括总生存以及局部无复发生存。研究共纳入701例患者,随机分为ME联合LLND组(n=351)和ME组(n=350)。ME联合LLND组和ME组5年无复发生存率分别为73.4%和73.3%。ME联合LLND组和ME组5年总生存率和5年局部无复发生存率分别为92.6%,90.2%和87.7%,82.4%。ME联合LLND和ME组出现局部复发的患者分别为26例(7.4%)和44例(12.6%)
文章最后认为,尚不能确认单纯直肠系膜切除术非劣效于直肠系膜切除术联合侧方淋巴结清扫。与单纯直肠系膜切除术相比,直肠系膜切除术联合侧方淋巴结清扫局部复发率更低,尤其是在盆腔侧壁。
【4】Cancer:研究证实吸烟会导致直肠癌死亡率增加!
迄今为止,直肠癌的五年存活率依然不到60%,探明可变的预后因素就显得尤为重要。曾有一些研究表明吸烟和直肠癌存活之间的关系,然而却都受限于相对较小的样本量和证据的不稳定性,不能得出明确的结论。在这项大规模人群队列研究中,研究人员就吸烟是否能成为一个独立的直肠癌生存率预后因子,及是否会因为性别、年龄和治疗方案而发生变化等做出了详尽深入的研究。
从美国国家癌症患者资料库中提取的1994到2012年间直肠癌(ICD10 C19-20)患者资料被用于此项研究,并就诊断时的吸烟状况做了分类,还对患者进行了5年随访工作。对不同组别(目前吸烟、戒烟、不曾吸烟)的直肠癌死亡率进行了多元变量Cox比例风险回归模型分析,还根据年龄细分了亚组,对诊断、治疗和性别等因素也进行了分析。
研究队列一共包含了10,794名直肠癌患者。在确诊时,25%的人吸烟,24%已经戒烟,剩余的从未吸烟。与从未吸烟的组别相比,吸烟者的癌症死亡率显着升高(HR, 1.15; 95% CI, 1.06-1.24),而已经戒烟的患者并没有表现出明显的变化(HR, 1.02; 95% CI, 0.94-1.11)。相较于女性患者(HR, 1.05; 95% CI, 0.90-1.23),这种吸烟与癌症死亡率的相关性在男性中表现的更加明显一些(HR = 1.13, 95% CI, 1.02-1.24),但是他们之间的相互作用并不显着(P=0.75)。吸烟对死亡率的影响也不会随年龄、切除手术、放化疗等而改变。
分析结果表明,直肠癌患者吸烟与癌症死亡率增加在统计学上具有显着相关性。
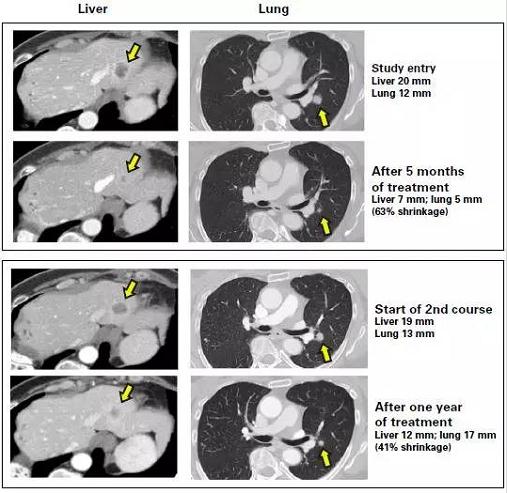
【5】ASCO2017:维生素D也是宝!高剂量维生素D或延缓转移性结直肠癌进展
一项由Dana-Farber癌症研究所研究人员开展的一项多机构的维生素D随机、单盲治疗癌症患者临床试验发现,高剂量微生物或可减缓转移性结直肠癌患者的疾病进展,相关研究结果发表在6月2-6日在美国芝加哥举行的第53届美国临床肿瘤学会年会(ASCO)上。
Dana-Farber胃肠道肿瘤学研究中心的主任Kimme Ng博士表示:“直至开展了这一研究才发现维生素D与转移性结直肠癌之间的关系”。 Ng博士将在ASCO会议上介绍SUNSHINE研究的早期成果。与此同时,患者可以与医生沟通检测其血液中维生素D的含量,并考虑服用补充剂维持血液中的剂量。
Ng博士表示这些研究数据需要在较大的研究中得到确认,但是对于转移性结直肠癌患者,采用高剂量维生素D与标准治疗方式相结合的方式似乎是有益的。
研究人员对139例接受化疗和贝伐珠单抗联合治疗的患者进行了临床试验。然后将患者随机分配到高剂量维生素D(8000单位/天,持续2周,每天三次,后续进行8000单位/天的治疗),或者每天服用400单位(通常由多种维生素丸提供的水平)作为对照组。
服用高剂量的结直肠癌患者疾病发生进展前中位数为13.1个月,对照组为11.2个月。在转移性癌症患者的世界里,2个月的差距是非常大的。建立补偿模型以消除年龄及先前存在的疾病情况等影响因素,在大约17个的中位随访期间,高剂量组的患者无进展生存期提高了33%。
其他试验结果表明,接受高剂量维生素D的患者比接受低剂量维生素D的患者更易经常发生腹泻。这种差别还没有达到统计学意义,可能与SUNSHINE试验中患者数量相对较少,高剂量组的患者更多的进行了手术驱除转移性肿瘤,也可能会有助于患者疾病的治愈。但是临床试验观察分析表明,血液中维生素D水平的较高的患者其无进展生存期和总生存期明显更好。
这项研究成果还需要更大型的研究来验证。基于以上研究结果,研究人员认为III期临床研究是必要的。
【6】Lancet Gastroen Hepatol:观察等待疗法可否有效治疗直肠癌?
对于新辅助化放疗后临床完全缓解的患者实施观察等待疗法(watch-and-wait)可以避免常规手术增加直肠癌病情加重的风险。但是,这种方法的安全性还不清楚。基于此,该研究评估了观察等待疗法治疗直肠癌的有效性和可靠性。
该研究系统地搜索MEDLINE,Embase和the grey文献(截至2016年6月28日)研究直肠癌患者经过新辅助化放疗产生临床反应后,在观察等待疗法治疗下的反应。该研究调查了在实施观察等待疗法后的肿瘤2年本地再生长的比例。通过研究比较实施观察等待疗法的患者、检测到临床完全反应后进行根治性手术的患者和表现直肠癌病理完全反应的患者的后期状况,评估了相关的非再生长复发,癌症特异性死亡率,无病生存率和总体生存率。
该项目建立了23项实验,共有867例平均随访12-68个月的患者。汇总的2年本地再生长为15.7%(95%CI 11·8-20·1); 其中95.4%(95%CI 89·6-99·3)的再生长患者进行了抢救治疗。临床完全缓解后观察等待疗法治疗患者与初次发病患者切除病理完全缓解后体征无显着差异(风险比[RR] 1·46,95%CI 0· 70-3.05)、癌症特异性死亡率(RR 0·87,95%CI 0·38-1·99)。组间总生存率差异无统计学意义(风险比[HR]0·73,95%CI0·35-1·51),手术组无病生存率较好(HR0.47,95 %CI 0·28-0·78)。研究人员发现,在watch-and-wait治疗的患者与接受手术治疗的临床完全缓解患者中各研究项目均无明显差异:非再生复发(RR 0。58,95%CI 0·18-1·90),癌症 - 特异性死亡率(RR 0·58,95%CI 0·06-5·84),无病生存率(HR0.56,95%CI0·20-1·60)或总生存期(HR 3·91 ,95%CI 0·57-26·72)。
该研究得出结论,大多数通过观察等待疗法治疗的患者无需再进行根治性手术,而那些肿瘤再生长的患者几乎都接受了救助治疗。虽然我们发现在观察等待疗法与手术治疗的患者中,非再生长性癌症复发或总体生存率没有显着差异,但统计案例过少,因此需要更多的前瞻性研究来确认观察等待疗法的长期安全性。
【7】Gastroenterology:饮食与结直肠癌风险
饮食质量指标评估(DQIs)主导的健康饮食可降低白种人结直肠癌风险。近日研究人员考察了4种DQIs指数(健康饮食指数2010 [HEI-2010],改变的健康饮食指数2010 [ AHEI-2010 ],改变的地中海饮食评分[aMED]以及预防高血压的膳食方法得分)在不同人种中对于结直肠癌风险评估的差异。
研究人员分析了190949份来自于非洲裔美国人,夏威夷土着人,日裔美国人,拉美裔和白人的数据,参与者年龄45-75岁,平均随访16年,发生4770例侵袭性结直肠癌。
研究发现4项DQIs分数与结直肠癌风险负相关,分数越高结直肠癌风险越低(P≤ 0.003)。调整后女性的AHEI-2010和aMED分数与肠癌风险相关性较低;男性HEI-2010调整后的风险比为0.69,女性为0.82 ; AHEI-2010男性调整后的风险比0.75,女性为0.90 ;aMED男性调整后的风险比0.84,女性为0.96;预防高血压的膳食方法得分男性调整后的风险比0.75,女性为0.86。所有指数分数仅与左结肠和直肠癌具有相关性,非裔美国人与其他4个族裔群体相比,指数分数与癌症风险相关性较差。
研究表明,饮食质量指标评估适用于绝大部分族裔群体的结直肠癌风险评估。
【8】Gut:肠道微生物标记有望诊断结直肠癌
根据一项最新研究结果,肠道菌群中的某些菌株与结直肠癌相关,可以作为一种非侵入性、准确、节约成本的诊断试验。“虽然之前已有研究发现肠道菌群与结直肠癌之间的关系,但研究结果未达成一致。据我们所知,我们的研究首次尝试收集现有的微生物标记基因数据并统一处理,” 德克萨斯大学公共卫生学院Manasi S. Shah博士说。“尽管队列人口、实验室方法和后续分析有统计学差异,对微生物结果有影响,令人鼓舞的是,我们发现细菌信号显着与大肠癌相关。”
Shah及其同事对2012年到2016年之间发表的9项研究进行了荟萃分析,采用不同的实验方法来评估结直肠癌和肠道微生物之间的关系。为了识别一组共同的特征性微生物标志物,他们评估了来自不同种族人群509份粪便样本的原始16S rRNA基因序列数据(79例大肠腺瘤,195例CRC,235例对照者)。他们还比较了两种不同的生物信息学方法以处理数据:常用的封闭参考操作分类单元分配方法,以及新型菌株特异性方法。与CRC有关的的特定微生物菌种包括Parvimonas MICRA ATCC 33270,咽峡炎链球菌和几种变形菌门。整个研究中,与对照组相比,这些在来自CRC患者的粪便样本中“频繁和显着增加”。与对照分类相比,使用这些微生物标志物分类显示,封闭参考操作分类单元分配方法AUROC为76.6%,菌株特异性方法80.3%。当结合微生物标志物与临床特点、分类准确率超过80%,两种方法的AUROC分别为83.3%和91.3%。
“微生物研究为先进的诊断和治疗提供了巨大的潜能。对于某些疾病,确定微生物为基础的联系已经相对简单。然而,对于大多数人,研究界仍然是通过筛查我们设法了解的有关微生物如何影响疾病发生和进展、为我们提供快速、准确诊断的数据,”贝勒医学院病理学和免疫学助理教授Emily B. Hollister博士说。“微生物与结直肠癌联系统一模式的识别代表了这些努力的重要一步。”
【9】AACR2017:膳食纤维增加,减少结直肠癌风险
一项发表在美国癌症研究协会(AACR)2017年度会议上的最新研究显示:饮食控制干预的目标是通过三餐和零食中米糠(RB)和菜豆粉(NB)的额外摄入,增加膳食纤维量,改变肠道菌群,从而可能降低结直肠癌风险(CRC)。来自科罗拉多州立大学的主要研究者Eric Borresen表示,米糠和菜豆含有高膳食纤维和其他重要植物化学物质,动物和人类流行病学研究中表明其可抑制结肠癌的发生。
该试验项目是富含豆类/麸皮营养的饮食肠道健康试验(BENEFIT)的一部分,试验旨在提高社区对此类知识的认知度,如如米糠、菜豆等简单的食物,如何影响肠道健康。
研究招募了29名CRC幸存者,随机分配接受4周不同的饮食计划,包括30g米糠+35g菜豆粉/天,或不含这些食物的控制饮食。米糠作为米的一部分,在加工过程中通过抛光去除。而试验中,米糠和菜豆粉在正常三餐和零食中都有提供。空腹血液、尿液和粪便样本分别在基线时间、第2周和4周时收集。RB或NB的消耗量(占每日热量摄入的4%~9%)带来膳食纤维,铁,锌,硫胺素,烟酸,维生素B6,叶酸和α-生育酚等摄入的增加。
在粪便微生物检测中,与对照组相比,补充饮食组的几种细菌的显着增加,包括甲烷短杆菌,瘤胃球菌,普氏杆菌和双歧杆菌。补充饮食组中的粪便微生物检测显示细菌的丰富性和多样性增加。血浆、尿液和粪便代谢组的变化,显示了一定数量的微生物,宿主和饮食衍生代谢产物的增加,如植物甾醇、脂肪酸、氨基酸、胆汁酸和碳水化合物代谢的小分子副产物。CRC预防方面,相比于对照组,在受试者接受膳食纤维补充饮食4周后,粪便代谢物提取物中CRC细胞发育减少。以上结果支持膳食RB/NB调节肠道新陈代谢,改变菌群,有可能降低结直肠癌风险。
【10】JAMA Surg:直肠癌:开腹手术可能比腹腔镜手术更好
直肠癌是消化道最常见的恶性肿瘤之一。直肠癌发病位置低,容易被直肠指诊及乙状结肠镜诊断。但因其位置深入盆腔,解剖关系复杂,手术不易彻底,术后复发率高。手术是治疗直肠癌的主要手段,遵循的原则是将肿瘤及其周边组织(直肠系膜)全部切除。直肠癌的预后与手术的成功与否有很大关系,实现肿瘤完整切除并且切缘阴性是非常重要的。
一项近期的法国研究数据汇总显示,与开腹手术相比,腹腔镜手术后出现直肠肿瘤不完全切除的可能性更大。该研究团队对14个随机对照试验的病理数据进行meta分析,以对比腹腔镜手术与开腹手术病理结局,研究结果在线发表在JAMA Surgery上。研究结果显示,相比于开腹手术,腹腔镜手术后的切缘阳性率和肠系膜不完全切除的概率均更高。全直肠系膜完整切除与切缘阴性为手术的主要目标。该Meta分析结果表明,腹腔镜手术可能不足以达到这一结果,这可能因为腹腔镜直肠癌切除术要求技术高,并极具挑战性。
现如今处于微创手术的时代,腹腔镜手术被认为是结肠癌手术的金标准,然而该研究表明,其在治疗直肠癌的中地位有很大争议。所以,关于腹腔镜手术治疗直肠癌的问题结果仍是开放的,需要有进一步的证据能够证明手术完整切除对于长期生存的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习一下很不错
64
学习一下很不错
68
#结直肠#
31
#研究进展#
37
文章真好.值得分享
69
不错的文章不错的文章
61
希望彻底治疗直肠癌
71
学习了谢谢分享
34
肠道菌群越来越受关注
30
DII应该可以用于许多研究
37