JAHA:年轻女性血红蛋白浓度变化与心血管风险和全因死亡率的关系
2018-08-16 xing.T MedSci原创
由此可见,这些研究结果表明定期进行Hb检查可能有助于识别有AMI、卒中、脑血管疾病和全因死亡风险的年轻女性。
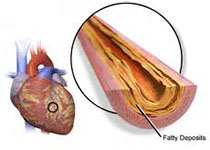
贫血被认为会增加高危人群的死亡风险,但其影响尚未在年轻人群中进行检验。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在确定血红蛋白(Hb)浓度及其变化对年轻女性急性心肌梗死(AMI)、卒中、脑血管疾病和全因死亡风险的影响。
研究人员分析了韩国国家健康信息数据库中808143名年龄在20至39岁但没有任何心脑血管疾病女性的数据。2年内Hb浓度增加一倍和Hb的变化作为研究暴露量。参与者的中位随访时间为10年,以确定AMI、卒中、脑血管疾病和全因死亡的风险。
通过分析,研究人员发现Hb浓度或Hb变化与AMI、卒中、脑血管疾病和全因死亡之间存在U形或J形关联。将Hb浓度从正常浓度增加至高浓度会增加了AMI的风险(风险比[95%置信区间]为1.49 [1.08-2.04])。对于卒中风险,将Hb浓度从正常浓度增加到高浓度会增加卒中的风险(风险比[95%置信区间]为1.10 [1.02-1.35]),并将Hb浓度从高浓度降低到正常范围会降低卒中的风险(风险比[95%置信区间]为0.80 [0.60-0.97])。将贫血症状改善,使Hb恢复至正常范围可降低全因死亡率(风险比[95%置信区间]为0.81 [0.69-0.94]); 然而,Hb浓度过度校正(Hb≥14.0g/dL)并不能显著降低全因死亡率。
由此可见,这些研究结果表明定期进行Hb检查可能有助于识别有AMI、卒中、脑血管疾病和全因死亡风险的年轻女性。
原始出处:
Gyeongsil Lee.et al. Association Between Changes in Hemoglobin Concentration and Cardiovascular Risks and All‐Cause Mortality Among Young Women.JAHA.2018. https://www.ahajournals.org/doi/full/10.1161/JAHA.117.008147
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管风险#
0
学习了
75
#全因死亡率#
24
#AHA#
30
#年轻女性#
26
#浓度#
25
学习!
72
学习了
48