Nature:阻断CAR-T“杀人风暴”!大牛团队揭示致命性细胞因子风暴缘起,现有高血压药物或可预防
2018-12-24 奇点糕 奇点网
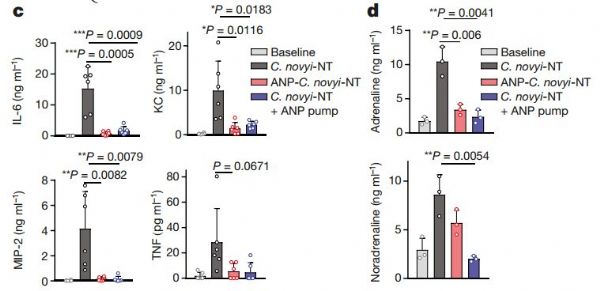
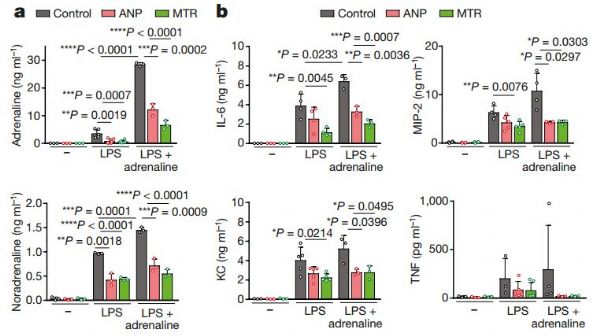
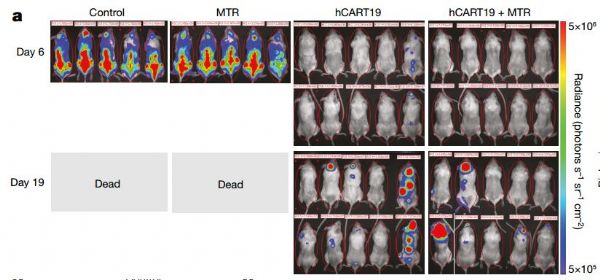
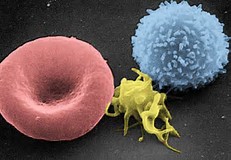
近期《自然》杂志上刊登了一项来自约翰·霍普金斯大学团队的成果,研究者们发现细胞因子释放与肾上腺素等儿茶酚胺类物质有关,限制其合成可以有效控制CRS发生!在多种免疫治疗癌症的小鼠模型中,这种方法都能够降低细胞因子产生、增加存活率,同时并未影响到治疗效果。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
35
#CAR-#
30
#胞因子#
25
#阻断#
29
#细胞因子#
22
学习了谢谢
65
好的很
62