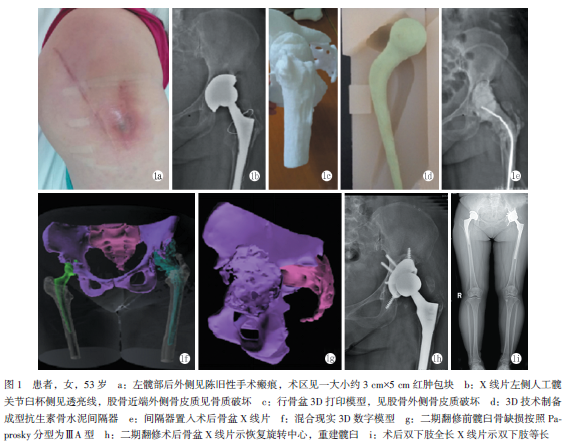
3D技术应用于髋关节布鲁氏菌感染二期翻修术1例
2019-06-10 马永光 孙立 李森磊 中国矫形外科杂志
患者,女性,53岁,左髋关节翻修术后6年,疼痛3个月,红肿2周。查体:左髋部后外侧见长约10CM及22CM陈旧性手术瘢痕,术区见一大小约3CM×5CM包块,皮温高,可触及液波感,左髋部4字征阳性,左髋活动受限。实验室检查:CRP:9.77mg/L,ESR:48mm/h,SPECT/CT结果示:见假体松动核浓聚考虑感染,结核三项、PPD、结核T-sport阴性,左髋穿刺行血培养瓶培养结果为布鲁氏菌。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#3D技术#
42
#布鲁氏菌#
23
#翻修术#
29
#3D#
27