Eur Respir J:系统性红斑狼疮相关性肺动脉高压患者的长期预后
2019-02-15 xing.T 网络
由此可见,TGA与患者长期存活相关,支持对SLE相关PAH患者进行治疗目标策略。基础心脏功能预测SLE相关PAH患者的生存和治疗目标。基线时患有浆膜炎的患者倾向于从强化免疫抑制治疗中获益并且具有更好的临床结局。
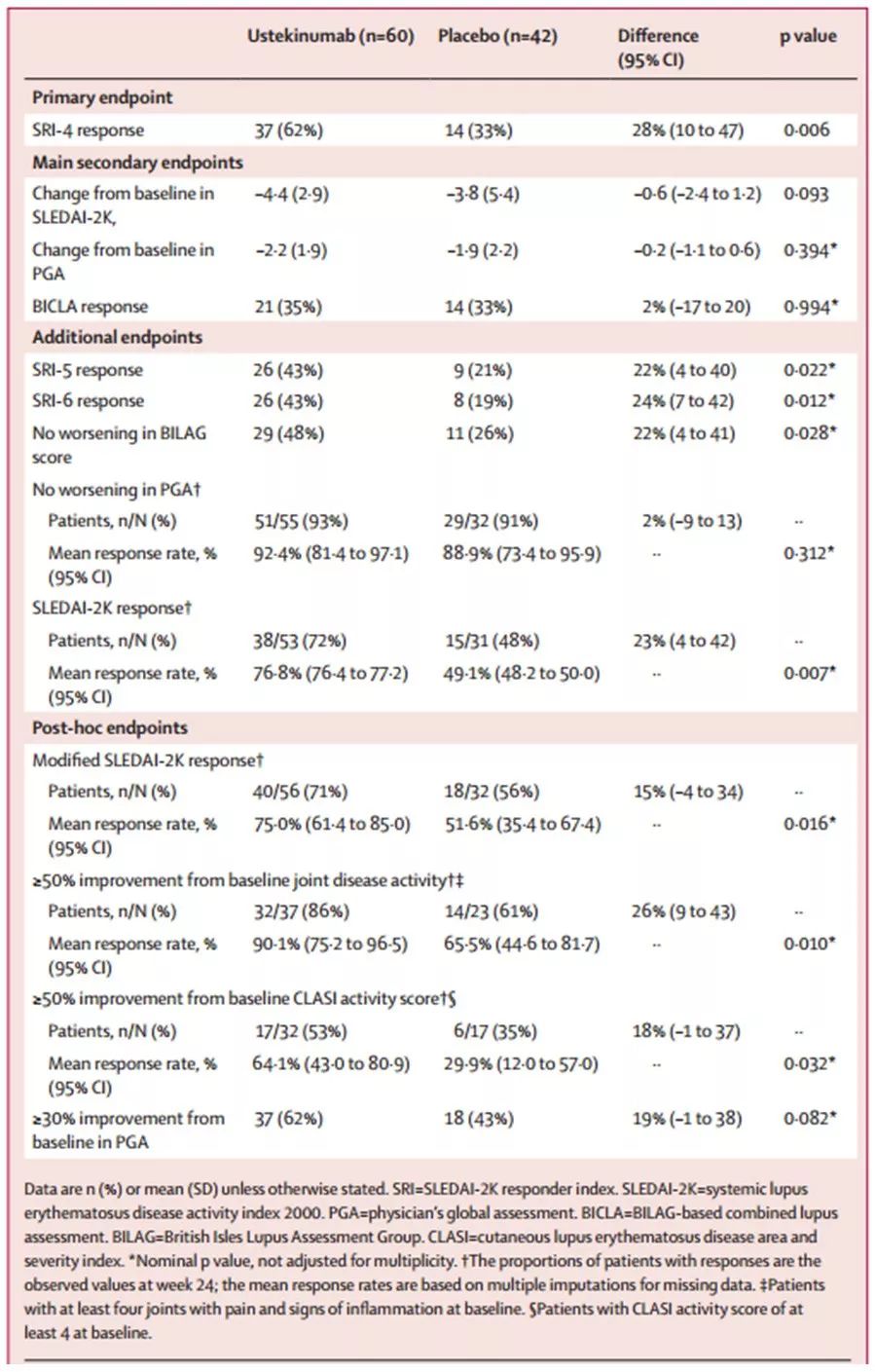
近日,呼吸疾病领域权威杂志Eur Respir J上发表了一篇研究文章,研究人员旨在确定右心导管检查确诊的系统性红斑狼疮(SLE)相关肺动脉高压(PAH)患者的长期临床结局和预后因素。
研究人员建立了一个SLE相关PAH的多中心前瞻性队列。收集了参与者的基线和随访记录。该研究的主要终点是死亡。次要探索终点是实现治疗目标(TGA),定义为综合结局。
该研究共有来自14个PAH中心的310名患者入组。参与者1年、3年和5年生存率分别为92.1%、84.8%和72.9%。1年、3年和5年的TGA率分别为31.5%、53.6%和62.7%。基线浆膜炎、6分钟步行距离>380米、心脏指数≥2.5L·min-1·m-2被确定为TGA的独立预后因素。在强化免疫抑制治疗后,患有基础浆膜炎的患者更有可能达到TGA。TGA被确定为SLE相关PAH患者生存的阳性预测因子。
由此可见,TGA与患者长期存活相关,支持对SLE相关PAH患者进行治疗目标策略。基础心脏功能预测SLE相关PAH患者的生存和治疗目标。基线时患有浆膜炎的患者倾向于从强化免疫抑制治疗中获益并且具有更好的临床结局。
原始出处:
Junyan Qian,et al.Long-term prognosis of patients with systemic lupus erythematosus-associated pulmonary arterial hypertension: CSTAR-PAH cohort study.Eur Respir J.2019. https://erj.ersjournals.com/content/53/2/1800081
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#相关性#
20
#肺动脉高压患者#
22
#系统性#
23
#长期预后#
18
#动脉高压#
26
#狼疮#
23
#红斑#
0
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
54