右侧颞部不明包块病例讨论
2018-05-19 Magic 医学界影像诊断与介入频道
患者男性,45岁,患者自诉18年前头顶部一约豌豆大小包块,无压痛,病史中包块无回缩,无破溃、出血、坏死等症状,当时未予重视,现包块逐渐长大,长约7cm的不规则包块,为进一步诊断来我院就诊治疗。
病历资料
患者男性,45岁,患者自诉18年前头顶部一约豌豆大小包块,无压痛,病史中包块无回缩,无破溃、出血、坏死等症状,当时未予重视,现包块逐渐长大,长约7cm的不规则包块,为进一步诊断来我院就诊治疗。
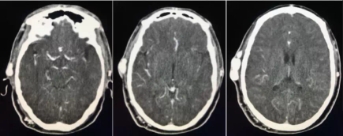
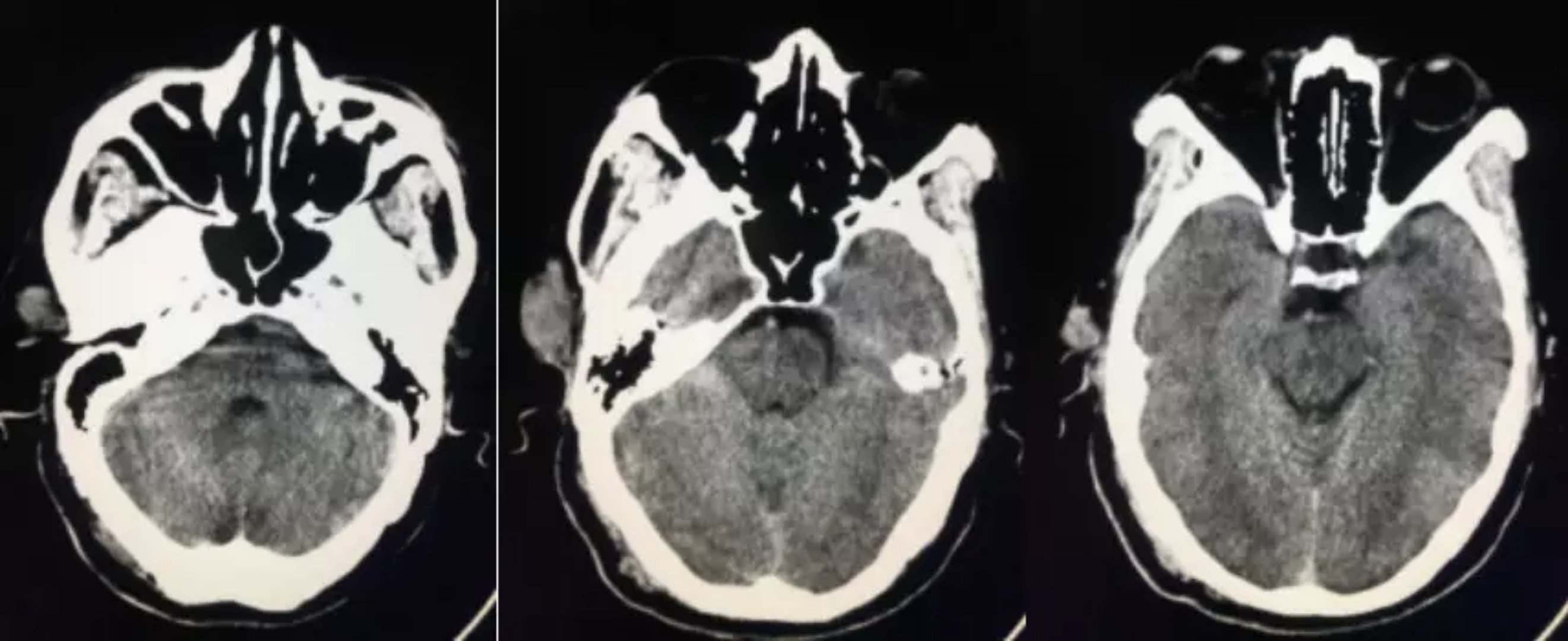
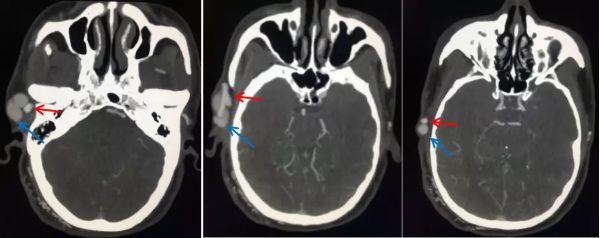
先看一下头颅CT平扫:
当时单纯从CT平扫来看,我们只是考虑了右侧颞顶部包块,建议进一步检查。
后来患者行头颅平扫+增强检查,动态增强后发现,我们都错了。
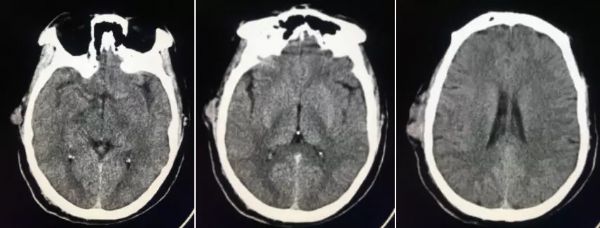
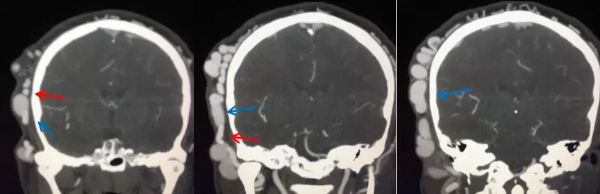
下面一起来欣赏一下增强检查的图像:
可以看到,右侧颞顶部包块动态增强是明显强化的,看到这里我想大家都应该往血管来源病变考虑了。
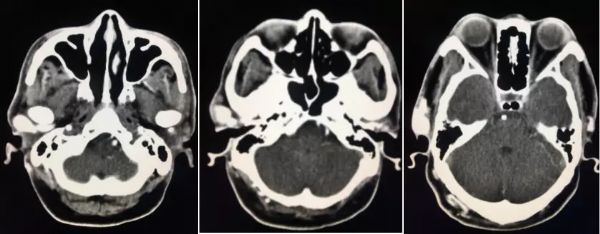
再来看下后处理MIP图像:
MIP处理发现右侧颞顶部包块,其实是异常增粗的血管影,仔细观察图像,发现是右侧颞浅动脉(红箭)和颞浅静脉(蓝箭)异常增粗、走行迂曲(犹如方便面)。
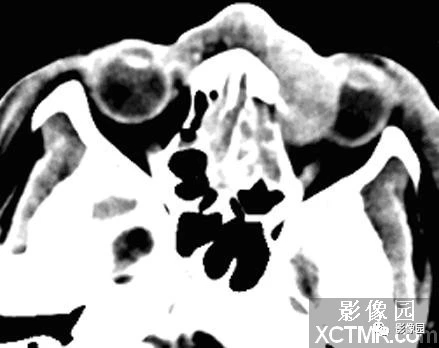
经过后处理曲面重建(CPR)发现在颞顶部异常增粗的颞浅动静脉有异常沟通(红色圆圈内),来张大图一起欣赏下:
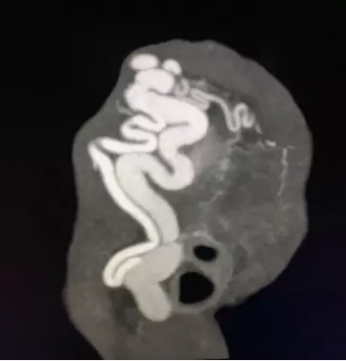
这下大家一看恍然大悟了吧,原来是右侧颞顶部的包块,是异常增粗的动脉静脉,居然是动-脉静脉瘘。
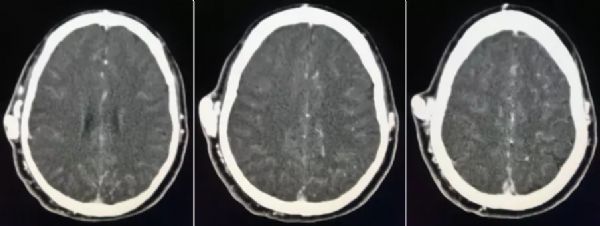
再来看以下更直观的图像,VRT图像:
这几张图看了以后,更直观的显示了异常增粗的动静脉,以及新生的异常发育蔓状血管,详细大家都清晰明了了。
这是一列典型的动-脉静脉瘘,只是发生在这个位置的少见一些,如果只是单纯的平扫,我想也很难确诊。所以,在现代的影像诊断中,一再强调综合诊断,单独的平扫往往不能明确诊断,需要增强检查,有些需要磁共振、超声、检查及临床的综合诊断。
讨论
这是一例典型的右侧先天性颞浅动脉-静脉瘘,颞浅动静脉瘘多为外伤性导致的,先天性的实属罕见。STA的AVF是罕见的病变,并且超过百分之九十五的这些病例是创伤后或医源性操纵的性质,并且遵循钝的,穿透性头部创伤。 STA的自发性AVF特别罕见,并且发表的报道很少。
AVF可以简单地由供血动脉和引流静脉之间的直接连接构成,而不需要插入毛细血管床,或者可以由于存在动脉瘤静脉曲张。 最主要的临床表现是出现伴有耳鸣和耳鸣的搏动性病变。 肿块可伴有头痛,头晕或出血。 体格检查揭示了一个明显的快感,连续的结痂和扩张的血管。 随着STA的近端压缩,脉动和兴奋通常减小或消失。
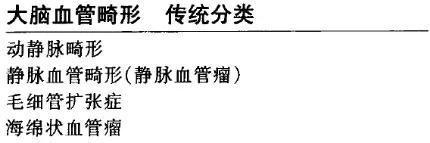
当有动脉及静脉有直接交通时即发生动静脉分流。这些分流可为丛状静脉畸形,也可为动静脉瘘道。一个动静脉畸形是一团发育不良的丛状血管,有一或数支供血动脉及一或数支引流静脉。动静脉畸形可有一单纯的丛状巢,或含一混合性丛状-瘘道巢。当一条洞穴动脉直接引流入一静脉通道而不伴有动静脉间的血管网时,便形成了动静脉瘘。动静脉瘘可单发或多发,可由一(单蒂的)或多个(多蒂的)供血血管供血。
病因
1.先天性动静脉瘘:是由胚胎的中胚层在发育演变过程中,动静脉之间残留的异常通道而引起。
2.后天性动静脉瘘:主要由外伤引起,包括贯通伤、挤压伤等(如各种穿刺伤,枪伤、钢铁和玻璃碎片飞击伤等)。受伤局部形成血肿,血肿机化后形成动静脉瘘的囊壁。
临床表现
急性后天性动静脉瘘可在受伤后立即出现,或者是在动静脉交通外填塞血块溶解后出现,在损伤局部有血肿,绝大多数有震颤和杂音。
慢性动静脉瘘病人的患肢肿胀、麻木、疼痛、乏力。在搏动性肿块局部有嗡嗡声。心力衰竭者可有胸闷、心悸、气急。常见体征有:
1.瘘区有杂音和震颤
不管动静脉瘘口径大小,在动静脉瘘部位都可以听到典型、粗糙而持续的隆隆声,称为“机器样”杂音。杂音在心脏收缩期增强,并沿着主干血管近侧和远端传导。这种杂音和假性动脉瘤引起微弱的舒张期杂音以及动脉狭窄引起的收缩期杂音鉴别。
2.脉率加快
这是由于静脉回心血量增加引起的Bainbridge反射或由于平均动脉压下降导致心脏工作量增加的结果。
3.心脏扩大和心力衰竭
由于大量血液经瘘孔迅速地流入静脉,静脉压增高,心脏的回流血量增加,引起心脏扩大。心脏进行性扩大可导致心力衰竭。心脏扩大和心力衰竭的程度与瘘口的大小,部位以及存在的时间长短有密切关系。越近心脏的瘘,如主动脉弓直接分支(颈动脉、无名动脉、锁骨下动脉)与伴行静脉形成的动静脉瘘,出现心力衰竭较早且严重。
4.局部升温
受累肢体在动静脉瘘部位表面皮温升高,高流速,动静脉瘘较远的部位皮温可能正常或低于正常。
5.静脉功能不全
动静脉之间直接交通,使静脉压增高。多数病人,动静脉瘘附近或远端的浅表静脉曲张。皮肤色素沉着,足趾或手指常发生溃疡,表现类似深静脉血栓后症状。
6.肢体远端缺血
多见于高流量分流的动静脉瘘,肢体远端血运减少导致缺血样体征。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#包块#
83
#病例讨论#
63
学习一下谢谢
82
学习
66