男性,11岁。
【主诉】
发现心脏杂音10年。
【现病史】
自幼发现心脏杂音,平时不易感冒,活动轻度受限,剧烈运动后感头晕等症状。患者嘴唇及四肢无发绀,无晕厥史,无四肢抽搐及蹲踞史,患者曾于2001年6月在我院全麻吸氧下行经皮肺动脉瓣球囊扩张术。2010年8月在我院复查超声心动图,诊断为“肺动脉瓣扩张术后再狭窄”,患者为求进一步治疗来我院就诊。患者近期无发热、咳嗽等症状,精神正常,饮食、睡眠可,大小便正常,体力及体重无明显变化。
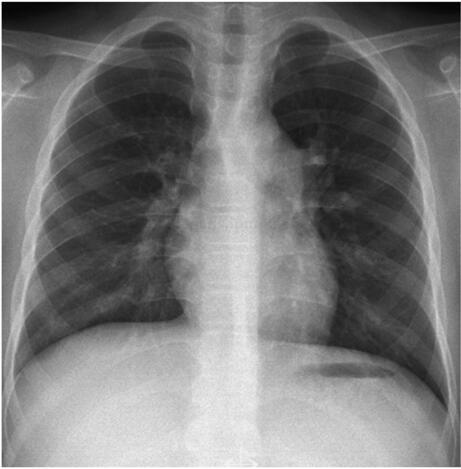
图101‐1 典型肺动脉瓣狭窄正位X 线胸片
【既往史】
否认肝炎、结核病史,无外科手术史及金属过敏史。
【查体】
T:36.1℃,P:72次/分,R:16次/分,上肢血压100/70mmHg,身高155cm,体重50kg。听诊于胸骨左缘2、3 肋间可闻及2/6 级收缩期杂音,P2 音偏弱,收缩期可触轻微震颤。余未发现其他阳性体征。
【辅助检查】
超声心动图示:右心房室扩大,右心室壁增厚,肺动脉瓣回声增强、瓣膜增厚、粘连,开放受限,闭合欠佳。估测肺动脉瓣跨瓣压差约64mmHg。诊断为“先天性心脏病、经皮肺动脉瓣球囊扩张术后再狭窄”。心电图示:“窦性心律,心电轴右偏”。X 线平片示:双肺血稍偏少,肺动脉段凸出,右心圆隆偏大(图101‐1)。
【入院诊断】
肺动脉瓣狭窄。
【治疗经过】
患者入院后完成必要的体格检查,完善术前的各种实验室检查。术前向患者及家属详细解释病情及手术情况,交代介入治疗的并发症及围术期的注意事项,取得患者及家属的同意,签署知情同意书,为介入治疗作好必要的准备。患者于2010年9月3日在局麻下行经皮肺动脉瓣球囊扩张术,其手术经过如下。
一、心导管检查与造影术
(一)消毒、铺巾
常规消毒右侧腹股沟区,消毒范围上至脐水平,下至膝盖上缘。常规消毒3 遍,于胸骨下缘放置标尺做标记。然后铺巾。
(二)穿刺
采用Sel dinger 技术穿刺右侧股静脉,插入6F 动脉鞘管以备用。
(三)术中造影及导管检查
首先送入6F 端侧孔导管行右心导管检查,测量肺动脉压、右心室压及肺动脉瓣跨瓣压差。然后送入5F 猪尾导管行右心室造影,测量肺动脉瓣环直径及观察瓣膜的运动情况,重要的是确定肺动脉瓣环的位置。本例患者肺动脉压24/13(16)mmHg,右心室压70/5(28)mmHg,肺动脉瓣跨瓣压差约50 mmHg(图101‐2),右心室造影可见三尖瓣少量反流,右心室扩大,肌小梁增粗,肺动脉瓣负影明显增厚,开放受限,可见圆顶征及喷射征,主肺动脉狭窄后扩张,右室流出道可见明显肌性肥厚(图101‐3、图101‐4),于舒张末期测量肺动脉瓣环直径约为21mm。
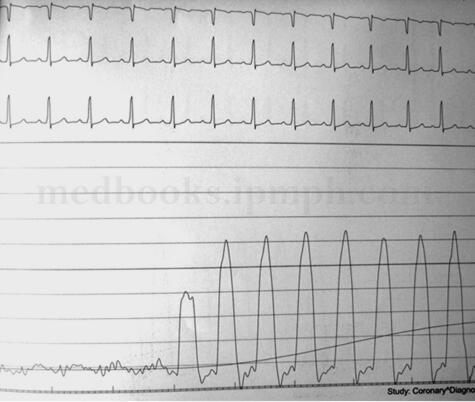
图101‐2 术前肺动脉瓣跨瓣压差
(四)扩张肺动脉瓣
首先将端侧孔导管送入肺动脉,沿端侧孔导管送入加长导丝(两圈半交换导丝)于肺动脉内,撤出端侧孔导管,用扩张管扩张皮肤、皮下组织及血管壁后,沿导丝送入扩张球囊行肺动脉瓣扩张治疗。扩张时先充盈前囊,后撤球囊导管至肺动脉瓣处,然后完全充盈整个球囊,使球囊腰部膨起(图101‐5、图101‐6)。本例患者选择直径26mm 的深圳擎源球囊分别以26mm、27mm 及27.5mm 直径扩张肺动脉瓣各1次,扩张成功。

图101‐3 右室造影收缩期图像,可见喷射征和右室流出道肌性狭窄

图101‐4 右室造影舒张期图像,可见圆顶征
(五)扩张后重复右心导管检查
扩张成功后,重复行右心导管检查,观察肺动脉瓣狭窄的缓解程度,本例患者扩张后肺动脉压26/10(18)mmHg,右心室50/1(16)mmHg,肺动脉瓣跨瓣压差约25mmHg(图101‐7)。

图101‐5 球囊扩张先充盈前球囊并后撤完全扩张

图101‐6 球囊卡于狭窄的肺动脉瓣后迅速完全扩张
二、中医药参与(包括术前和术后)
平素除感冒发热曾经用过中药或中成药外,未接受过专门的中医药治疗。
三、术后随访
患者于术后1、3、6个月随访,临床症状明显改善,活动量较前增加,心脏听诊仍可闻及(1~2)/6 级收缩期杂音,P2 不弱,收缩期震颤消失。复查超声心动图示心脏各房室内径值属正常范围,肺动脉瓣仍有增厚,开放轻度受限,关闭欠佳,肺动脉瓣狭窄明显减轻,肺动脉瓣少量反流,肺动脉瓣跨瓣压差约25mmHg,心电图同术前无明显变化,X 线平片示双肺血大致正常,主动脉结不宽,肺动脉段凸,心胸比0.46。

图101‐7 球囊扩张术后跨瓣压差下降,但仍有压差
【讨论】
肺动脉狭窄的球囊扩张是一种较为成熟的技术,自1986年引入我国,目前在国内一些大中型医院已广泛应用于临床,由于具有创伤小、恢复快及住院时间短等优点,其早已作为先天性肺动脉瓣狭窄患者的首选治疗方法。随着介入治疗器械的不断创新及国产器材的研发成功,介入治疗的水平在不断提高,而介入治疗的费用明显较低,现在肺动脉瓣狭窄球囊成形术的费用比手术费用还要低。
肺动脉瓣狭窄球囊扩张治疗的典型适应证是单纯肺动脉瓣狭窄,其肺动脉瓣跨瓣压差≥50mmHg。最佳的治疗年龄是2~4岁。随着介入治疗器械的改进及操作技术的提高,其介入治疗的适应证范围也明显扩大,目前,肺动脉瓣狭窄介入治疗的适应证已扩大到肺动脉瓣狭窄之跨瓣压差≥30mmHg 的患者及肺动脉瓣狭窄合并其他适宜作介入治疗的先心病复合畸形患者等。
本手术虽为较为安全有效的治疗肺动脉瓣狭窄的微创治疗方法,但是仍有5%左右的并发症,总体死亡率<0.5%,多见于新生儿、小婴儿等重症病例。常见的并发症除心导管术以外的并发症外,还有扩张时一过性血压下降、心律失常(包括心动过缓、传导阻滞等)、血管损伤及三尖瓣关闭不全、心脏穿孔及心包填塞等。本手术成功的关键是肺动脉瓣环直径的测量、扩张球囊直径的选择及球囊导管位置的正确定位。国外报道肺动脉瓣球囊成形术的再狭窄率约为10%,其主要原因是其扩张球囊直径选择得偏小,早年选择单球囊扩张的直径与肺动脉瓣环直径之比为1∶1.1。本例患儿发生再狭窄的原因也是因为当时球囊型号不全,直径偏小所致。目前,扩张球囊直径与肺动脉瓣环径之比以大于1.2、小于1.5为宜。现在,用于扩张二尖瓣狭窄的硅胶球囊已广泛应用于肺动脉瓣狭窄的介入治疗,尤其介入治疗器械的国产化取得明显的进展,国产小儿型硅胶瓣膜扩张球囊已可以用于3岁左右(或体重15~20kg 以上)的患儿。
本例由于右室流出道肥厚较明显,故其肺动脉瓣虽然完全张开,但流出道狭窄的恢复仍需一定时间,甚至变化不明显。肺动脉瓣狭窄球囊扩张术后,心脏杂音均会有所改善,但多半仍可闻及轻度收缩期杂音,术前应向患者解释清楚,以免引起不必要的误会。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肺动脉瓣#
44
#球囊扩张#
37
#扩张#
28
#球囊#
45
学习一下谢谢
73
学习新知识了一谢谢
61