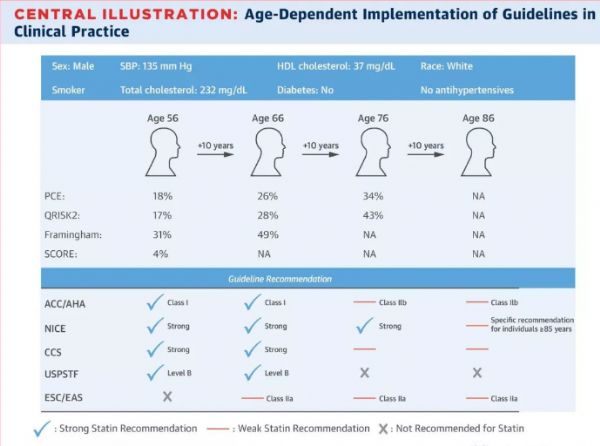
JACC:老年人群他汀一级预防六个问题,衰弱、合并症及多重用药的老年人须警惕不良反应
2018-01-09 卢芳 中国循环杂志
随着老龄化进程和人群寿命的延长,全世界≥65岁的老人越来越多,而动脉粥样硬化性心血管疾病(ASCVD)是主要的老年人群“杀手”。在美国,到2030年,ASCVD患病率将增加43%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#合并症#
38
#不良反应#
43
#JACC#
28
#ACC#
33
#老年人群#
34
^_^^_^^_^^_^
69
学习了.涨知识
62