Cell Stem cell:慢性粒细胞白血病体内的“钉子户”
2019-03-28 小通 生物通
最近发表在《Cell Stem Cell》杂志上的研究中,Ravi Bhatia博士和他在阿拉巴马大学、苏黎世大学和大阪大学的同事们描述了一种特定类型的骨髓细胞表达一种特定的趋化因子,控制这些抵抗治疗的静止的白血病干细胞。
最近发表在《Cell Stem Cell》杂志上的研究中,Ravi Bhatia博士和他在阿拉巴马大学、苏黎世大学和大阪大学的同事们描述了一种特定类型的骨髓细胞表达一种特定的趋化因子,控制这些抵抗治疗的静止的白血病干细胞。
大多数慢性粒细胞白血病患者可以用酪氨酸激酶抑制剂治疗,这些药虽然很有效,患者可以得到深度缓解和延长生存期,但是患者体内仍然存在着静止的白血病干细胞,因此他们必须继续这种抑制剂治疗以维持病情。
静止的白血病干细胞也被称为“休眠细胞”,存在于骨髓微环境,骨髓龛是维持正常造血干细胞的特定解剖位置。它们对慢性粒细胞白血病的白血病干细胞的维持作用尚不清楚。
最近发表在《Cell Stem Cell》杂志上的研究中,Ravi Bhatia博士和他在阿拉巴马大学、苏黎世大学和大阪大学的同事们描述了一种特定类型的骨髓细胞表达一种特定的趋化因子,控制这些抵抗治疗的静止的白血病干细胞。趋化因子CXCL12由特定的骨髓间质细胞表达,有研究证明间充质间质细胞有助于支持正常干细胞。
“已经接受酪氨酸酶抑制剂治疗的患者,其体内休眠的原始白血病干细胞的持续存在是治疗慢性粒细胞白血病的主要障碍,”Bhatia说。“这项工作确定了特定间充质间质细胞,龛细胞,负责维持白血病干细胞处于静止和治疗抵抗状态,并表明,靶向这些龛细胞相互作用可以激活白血病干细胞,使其对治疗敏感,增强药物清除能力。”
CXCL12在骨髓中表达并控制造血干细胞的维持。已知骨髓中有四种类型的细胞大量生产CXCL12。在小鼠实验中,Bhatia等人分别缺失每种细胞类型生产CXCL12的基因,然后观察每种类型的缺失如何影响白血病干细胞的调节。
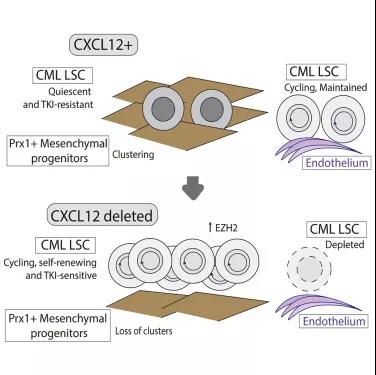
他们发现,删除间充质间质细胞CXCL12,增强了白血病的发展,降低了小鼠生存率,而其他三种表达CXCL12的骨髓龛细胞没有这种表现。原因是慢性粒细胞白血病干细胞增殖和细胞周期增加。但是,周期性白血病干细胞对酪氨酸激酶治疗变得敏感,可以导致清除率增加。
骨髓成像研究显示,间质细胞重新组织与白血病干细胞共同定位。缺失CXCL12后,间质细胞和白血病干细胞的共定位消失,进一步支持了CXCL12表达对维持白血病干细胞生态位的重要性。
“综上,结果表明,表达CXCL12的间充质间质细胞作为维持骨髓中静止、抵抗治疗的白血病干细胞的特殊调节龛位发挥作用,”Bhatia说。
与间充质间质细胞相比,骨髓微环境内皮细胞CXCL12表达的缺失导致慢性髓系白血病干细胞数量减少,并可以延长小鼠存活率。这表明,CXCL12表达内皮细胞龛帮助维持白血病干细胞。
细胞龛内的间充质间质细胞和表达CXCL12的内皮细胞对白血病干细胞具有明显不同的调节作用。
原始出处:Agarwal P1, Isringhausen S2, Li H1, et al. Mesenchymal Niche-Specific Expression of Cxcl12 Controls Quiescence of Treatment-Resistant Leukemia Stem Cells. Cell Stem Cell. 2019 Mar 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Cell#
24
#CEL#
32
#stem cell#
32
#STEM#
27