全国首例!介入机器人“鲁班”完成机器人辅助全脑血管造影手术
2020-01-03 杨雪(整理) 健康界
2019年12月19日,首都医科大学附属北京天坛医院(下称“北京天坛医院”)通过远程遥控手术机器人“鲁班”,成功为一名来自陕西的患者完成了全脑血管造影手术。这是我国首例机器人辅助全脑血管造影手术。该手术由北京天坛医院神经介入中心主任医师李佑祥、吕明指挥,副主任医师江裕华操作。建立血管通路后,江裕华来到手术室外的医生主操作端,通过操纵2个手杆,远程遥控介入机器人“鲁班”,精确实施了对患者左、右颈动脉
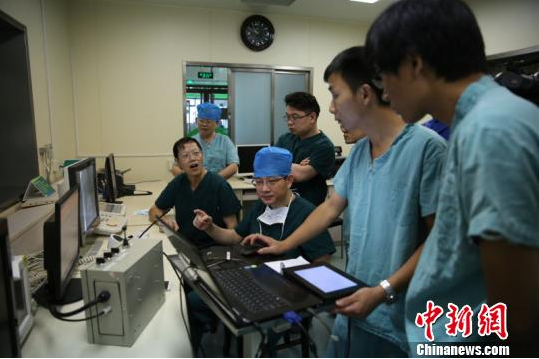
该手术由北京天坛医院神经介入中心主任医师李佑祥、吕明指挥,副主任医师江裕华操作。建立血管通路后,江裕华来到手术室外的医生主操作端,通过操纵2个手杆,远程遥控介入机器人“鲁班”,精确实施了对患者左、右颈动脉、锁骨下动脉、椎间动脉等血管的造影手术。手术中导管导丝递送、旋转顺畅稳定。检查结果显示动脉瘤栓塞完全,载瘤动脉通畅。
本次手术使用的“鲁班”微创血管介入手术机器人系统,由李佑祥教授的临床研究团队,联合北京理工大学肖楠教授的机器人技术团队共同研发,受国家重点研发项目支持,具有完全自主知识产权。项目实施过程中实现了对同构式多器械协同管丝递送、无菌隔离非固联传动等多项微创介入手术机器人的关键技术突破。
据李佑祥介绍,目前“鲁班”机器人系统的操作范围主要限于手术室外,随着5G技术的发展,未来将可实现跨地区远程手术。
据悉,李佑祥团队的“高精度微创血管介入手术机器人产业化及示范应用研究”项目于2017年11月获得科技部批准,旨在攻克血管介入手术机器人产业化过程中的关键技术,形成具有完全自主知识产权的国产高精度微创血管介入手术机器人产品,建立手术室内整体解决方案。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#机器人#
25
#造影#
36
#机器人辅助#
32
#脑血管造影#
52
#机器#
33