ASA 2015 知识更新(二十一)剖宫产手术麻醉的观点
2016-04-19 牛瑞斌 新青年麻醉论坛
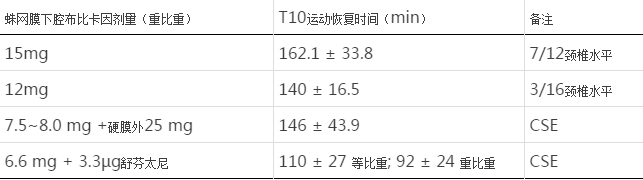
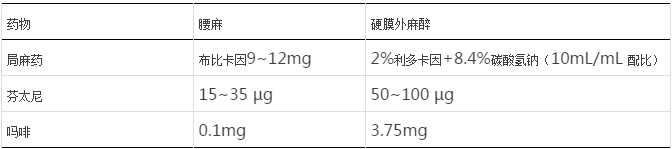
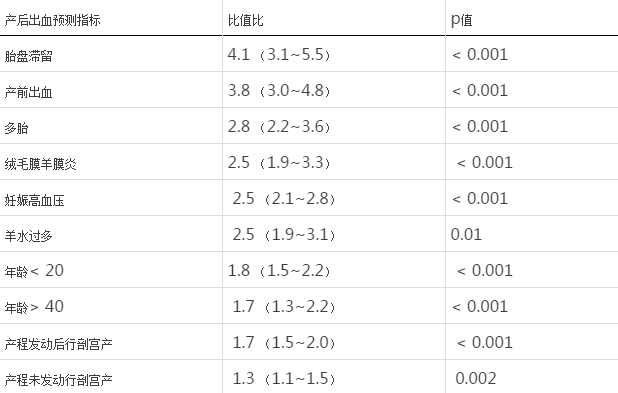
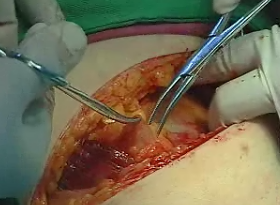
剖宫产手术麻醉的最新观点 ASA 2015 知识更新(二十一) 作者:Lawrence C. Tsen 剖宫产术可追溯到罗马皇帝尤利乌斯·恺撒时期(公元前100年),而他本人可能不是以剖宫产方式出生的。20世纪之前,产妇的死亡率都较高,而当今的发达国家中大约每3位产妇中就有1位通过剖宫产来进行分娩,这得益于外科及麻醉技术的发展、产钳使用的减少、臀位与复杂分娩的减少以及二次
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASA#
34
#手术麻醉#
41
文章不错,值得拜读
56
学习!
50
不错的文章!
98
文章不错
119
值得学习
85
实践出真知。
60