Lancet haemat:利妥昔单抗可显著降低滤泡性淋巴瘤向侵袭性淋巴瘤转化的风险
2018-07-05 MedSci MedSci原创
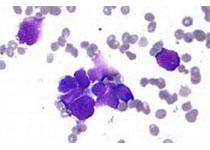
滤泡性淋巴瘤向侵袭性淋巴瘤转化,会严重影响患者预后。研究人员开展Aristotle研究对应用利妥昔单抗对组织学类型转化的风险及其预后的影响进行评估。本研究数据来源于欧洲的11个合作单位。研究对象为1997年1月2日-2013年12月20日期间经组织学确诊的年满18岁的滤泡性淋巴瘤(1期、2期或3a期)患者。组织学转化定义:一线化疗后活检发现侵袭性淋巴瘤。主要评估节点:组织学转化的累积风险和转化后的
本研究数据来源于欧洲的11个合作单位。研究对象为1997年1月2日-2013年12月20日期间经组织学确诊的年满18岁的滤泡性淋巴瘤(1期、2期或3a期)患者。组织学转化定义:一线化疗后活检发现侵袭性淋巴瘤。主要评估节点:组织学转化的累积风险和转化后的存活期。
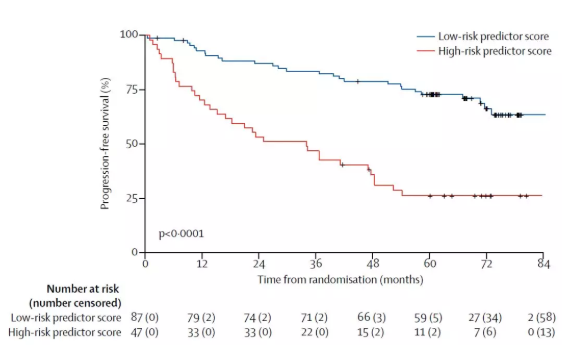
共筛查了10001位滤泡性淋巴瘤患者信息,其中8116位符合分析要求。509位发现组织学转化。中位随访87个月(1-222)后,组织学转化的10年累积风险为7.7%(95% CI 6.9-8.5)。采用利妥昔单抗治疗的患者组织学转化的10年累积风险为5.2%(95% CI 4.5-6.2),而未采用利妥昔单抗治疗的患者的是8.7%(7.2-10.6;风险比[HR]0.73,95% CI 0.58-0.90;p=0.004)。仅采用利妥昔单抗诱导治疗的患者和同时采用利妥昔单抗诱导和维持治疗的患者的组织学转化的10年累积风险分别是5.9%(95% CI 5.0-7.0)和3.6%(95% CI 2.3-5.5;HR 0.55,95% CI 0.37-0.81;p=0.003)。509位组织学转化的患者中死亡287位,转化后的10年存活率仅32%(95% CI 26-38)。转化之后是否采用利妥昔单抗治疗的存活率无明显差异。
应用利妥昔单抗可显著降低组织学转化的风险。
原始出处:
Massimo Federico,et al. Rituximab and the risk of transformation of follicular lymphoma: a retrospective pooled analysis. The Lancet Haematology. July 04,2018.https://doi.org/10.1016/S2352-3026(18)30090-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HAE#
27
#利妥昔#
28
#Lancet#
26
#滤泡性淋巴瘤#
37
#EMA#
33
#侵袭性#
34
学习
62