Ann Oncol:HER2+胃癌患者或是拉帕替尼治疗的获益人群
2018-02-25 肿瘤资讯编辑部 肿瘤资讯
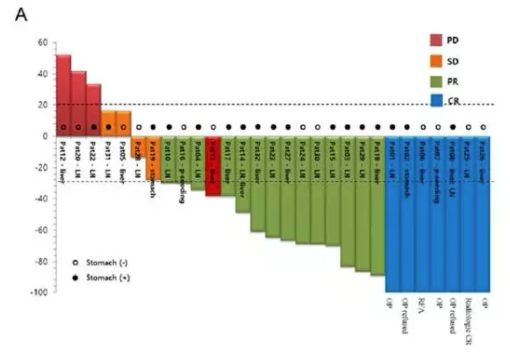
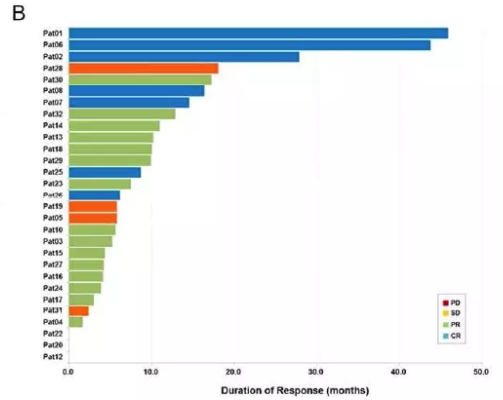
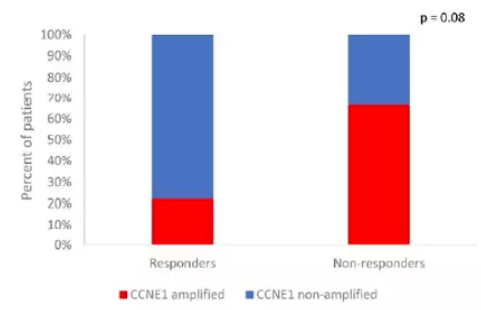
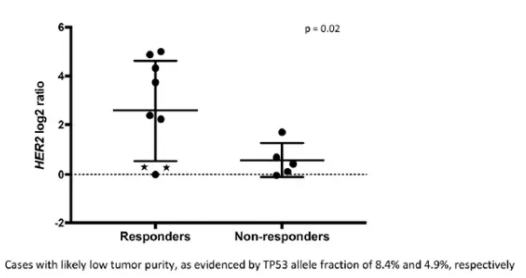
近日,《Ann Oncol》杂志在线发表的一项新研究,对应用拉帕替尼治疗的胃癌患者疗效进行探索分析,并对治疗期间基因组学层面的变化进行研究,以期得出可能对拉帕替尼疗效有潜在预测作用的生物标志物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胃癌患者#
33
#Oncol#
0
学习了
59
学习了
46
#拉帕替尼#
22
学习了.谢谢分享
58