Chest:慢性阻塞性肺疾病患者血清sirtuin-1下降
2017-05-19 xing.T MedSci原创
由此可见,血清中SIRT1(s120s)在COPD患者中有所降低,可能反映了降低了氧化应激细胞内的SIRT1,并可能作为COPD某些疾病特征的潜在生物标志。
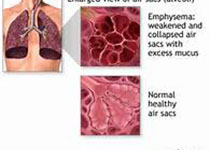
蛋白去乙酰化酶sirtuin-1(SIRT1)是一种抗衰老分子,在慢性阻塞性肺疾病(COPD)患者的肺脏中有所降低。近日,据报道血清中可以检测出SIRT1,但COPD患者血清中SIRT1水平尚未被报道。
研究人员通过Western blot方法测定了血清SIRT1,并通过阳性对照计算出了蛋白条带灰度值的相对比值。
通过Western blot方法定量的SIRT1有几个不同大小的分子量,包括120kda(实际大小)和片段(102、75kda)。其中,只有120kda血清SIRT1(s120s)在COPD患者中显著降低,相比于对照组无COPD的患者(健康者s120s比值:0.90±0.34 vs. COPD患者:0.68±0.24;P=0.014),并与气道阻塞(FEV1/FVC;R=0.31;P=0.020)及其预测的FEV1%测量的COPD严重程度呈正相关(R=0.29;P=0.029)。血清s120s也表现出与体重指数(R=0.36;P=0.0077)和肺脏每单位体积的扩散能力呈正相关(R=0.32;P=0.025)。它也随着肺气肿严重程度(R=-0.40,P=0.027)和频繁COPD恶化的临床病史(不频繁:0.76±0.20 vs. 频繁:0.56±0.26;P=0.027)明显降低。在正常培养条件下的A549细胞和原代上皮细胞的上清液中没有检测到SIRT1。
由此可见,血清中SIRT1(s120s)在COPD患者中有所降低,可能反映了降低了氧化应激细胞内的SIRT1,并可能作为COPD某些疾病特征的潜在生物标志。
Satoru Yanagisawa.et al.Decreased serum sirtuin-1 in chronic obstructive pulmonary disease.chest.2017.http://journal.publications.chestnet.org/article.aspx?articleid=2628645
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Chest#
19
#EST#
33
#疾病患者#
23
#阻塞#
22
谢谢!学习了!
70
谢谢分享
49