Pharmacoepidemiol Drug Saf:肝素诱导性血小板减少症:血栓栓塞并发症的风险因素是什么?
2017-11-02 王淳 环球医学
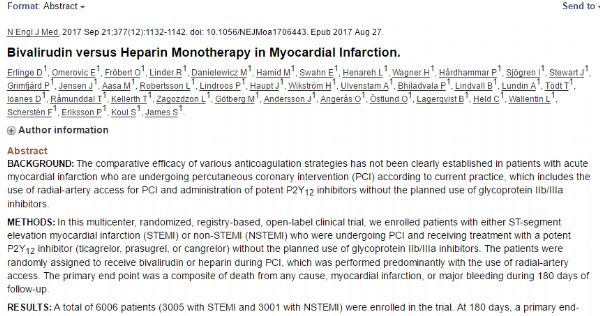
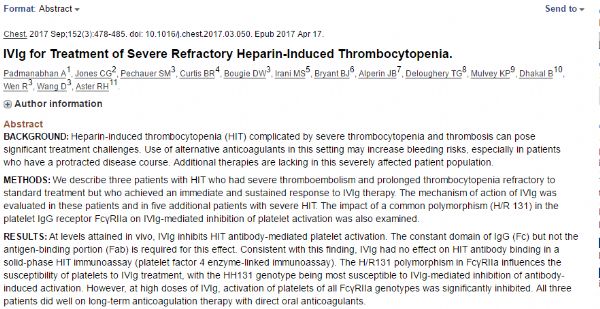
2017年10月,发表在《Pharmacoepidemiol Drug Saf》的一项由德国科学家进行的研究,考察了免疫介导的肝素诱导性血小板减少症(HIT2型,HIT)发生血栓栓塞并发症的相关风险因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Drug#
33
#诱导性#
38
#并发#
32
#Pharm#
22
#MAC#
38
#pharma#
33
#血栓栓塞并发症#
24
#肝素诱导性血小板减少症#
0
#血小板减少#
31
学习了受益匪浅
50