ASCO 2016:中国自主创新小分子靶向药物埃克替尼——CONVINCE研究结果揭晓
2016-06-06 佚名 中国医学论坛报
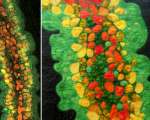
美国临床肿瘤学会(ASCO ®)年会系世界范围内最受关注、影响力最大的临床肿瘤学盛会,尤其在精准医疗等领域快速发展的今天,汇聚了最前沿学术进展、研究热点及诊疗技术的2016 ASCO ®年会更是声名赫赫、精彩纷呈。 在本届大会上,中国医学科学院肿瘤医院副院长石远凯教授就备受关注的CONVINCE研究做了相关报道,该研究系一项有关表
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#分子靶向药物#
40
#分子靶向#
47
#研究结果#
39
#小分子#
42
#ASC#
30
#小分子靶向药物#
44
#创新#
26
#埃克替尼#
40
这牛人啊
109
很有前途
101