Spine:手术时间是单节段腰椎术后并发症的独立危险因素
2014-06-04 佚名 丁香园
腰椎融合术是治疗腰椎不稳和慢性腰痛的常规术式。手术时间延长与并发症发生率增加以及死亡率的上升有关,但是并没有大范围研究来证明腰椎手术时间与术后并发症之间存在相关性。 美国芝加哥医学院的学者们通过多中心的回顾性研究来评价手术时间延长对单节段腰椎融合术后结果的影响。文章发表于2014年4月发表的Spine上。 研究者们从2006-2011年美国外科医师学会手术质量改善项目(NS
腰椎融合术是治疗腰椎不稳和慢性腰痛的常规术式。手术时间延长与并发症发生率增加以及死亡率的上升有关,但是并没有大范围研究来证明腰椎手术时间与术后并发症之间存在相关性。
美国芝加哥医学院的学者们通过多中心的回顾性研究来评价手术时间延长对单节段腰椎融合术后结果的影响。文章发表于2014年4月发表的Spine上。
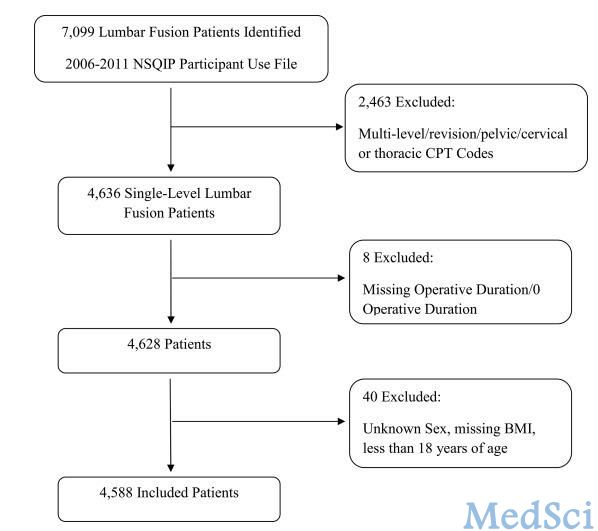
研究者们从2006-2011年美国外科医师学会手术质量改善项目(NSQIP)数据库中筛选出4588名患者纳入研究。手术时间分为五级: < 2、 2–2.99、 3–3.99、 4–4.99、 ≥ 5 小时。患者的人口统计学资料、医学合并症以及临床手术特点均被纳入数据分析。
将术后三十天并发症分为:总体并发症、外科并发症、内科并发症。外科并发症包括手术部位感染及伤口开裂。内科并发症为与外科因素无关的其他并发症。
在此之前,已有研究表明手术时间与术后并发症存在联系,但是手术时间与手术方式混杂,不能说明手术时间就是术后并发症的独立危险因素。本研究通过相同术式间比较(基于CPT编码)将手术时间独立出来进行分析。患者资料中存在统计学差异的变量,如年龄、BMI等通过多元logistic回归分析进行控制。
结果显示术后早期结果与手术时间存在显著的线性关系,并发症率随手术时间的延长而上升。进一步的分析显示手术时间仍是术后外科、内科及再次手术等并发症独立且显著的危险因素。
手术的麻醉分级(ASA分级)也与术后并发症相关,ASA 4级与ASA 3级均较ASA1/2级存在更大的术后并发症风险。手术方式同样与术后并发症存在相关性:后外侧入路发生外科并发症的发现更高,前路椎间融合提示更大的再手术率。
作者列举出之前学者们的研究结果,与本研究结果一致,均提示手术时间是腰椎融合手术的质量指标。手术时间的延长带来了更高的术区感染风险、DVT发生率、输血及输血并发症。
由此可见,手术时间的延长会增加单阶段腰椎融合术后并发症发生的风险,手术时间也成为评价手术技巧的衡量尺度。这就要求术者在围手术期做好充分准备,尽量缩短手术时间,最大限度减少术后并发症。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#并发#
38
#手术时间#
37
#Spine#
41
#独立危险因素#
31
#腰椎#
28