Blood:胞外组蛋白可增加红细胞的渗透脆性、诱导贫血。
2017-11-15 MedSci MedSci原创
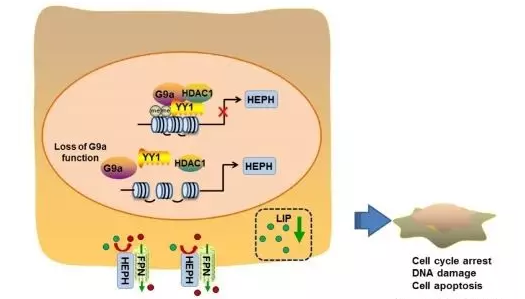
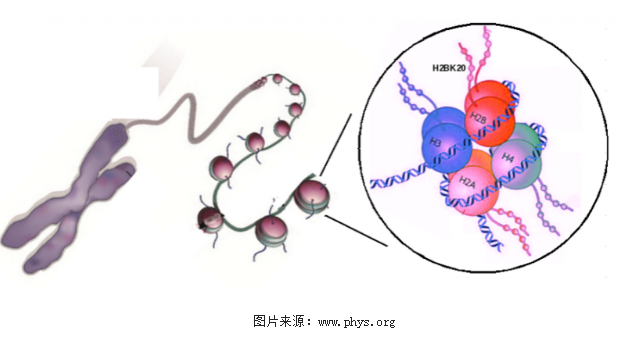
已发现细胞外组蛋白在多种疾病的发病过程中发挥重要作用,主要是通过其细胞毒性影响有核细胞,及其促进血小板激活导致血栓形成和血小板减少症的特性。但胞外组蛋白对于红细胞功能的影响尚知之甚少。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了谢谢分享!!
67
#红细胞#
39
#组蛋白#
0
学习了谢谢分享!!
84
谢谢.学习了
88
是很好的学习材料.不错.以后会多学习.
2
学习了.希望继续研究
64